KING ABDULLAH UNIVERSITY OF SCIENCE & TECHNOLOGY (KAUST)
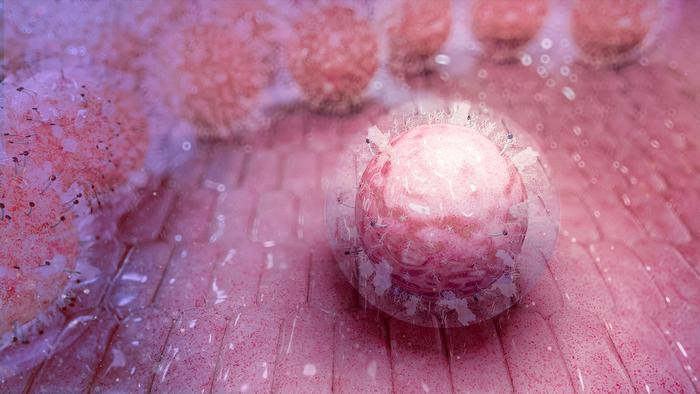
IMAGE:
RESEARCHERS HAVE IDENTIFIED A METHOD TO ENHANCE THE REGENERATIVE CAPABILITIES OF STEM CELLS FOUND IN UMBILICAL CORD BLOOD, WHICH COULD HAVE BENEFITS FOR BONE MARROW TRANSPLANTS.
view more
CREDIT: © 2024 KAUST; HENO HWANG.
A method that enhances the functionality of an often-overlooked type of stem cell could lead to better treatments for blood-related diseases.
“These cells could go a long way toward improving regenerative medicine,” says Jasmeen Merzaban, a biochemist at KAUST who led the research.[1]
In stem cell transplants — also referred to as bone marrow transplants — patients with malfunctioning bone marrow are infused with a new set of healthy blood-forming stem cells, known as hematopoietic stem cells (HSCs).
These cells have historically been identified by the presence of a protein called CD34. HSCs that express this surface marker are celebrated for their proficiency in homing to and establishing themselves within the bone marrow.
However, this emphasis on CD34-positive HSCs has inadvertently sidelined a population of CD34-negative counterparts — cells mostly found in umbilical cord blood that, although limited in their migration abilities within the bloodstream, are thought to have greater regenerative capacity because of their more primitive developmental state.
“There is deep untapped potential in using CD34-negative HSCs in transplantation,” says Asma Al-Amoodi, a postdoc in Merzaban’s lab. Along with her colleagues, she sets out to augment their therapeutic value.
The researchers first characterized the different populations of HSCs found in cord blood and noticed that CD34-negative cells were particularly lacking in sialyl Lewis X, a sugar molecule expressed by CD34-positive HSCs that helps direct the cells to the bone marrow.
To address this deficiency, the researchers treated CD34-negative cells in the lab with enzymes necessary to boost production of this sugar. The cells then gained newfound homing abilities.
After transplantation into mice, the souped-up CD34-negative cells quickly made their way into the bone marrow, where they continued to pump out new healthy blood and immune cells for months. The HSCs also showed elevated activity of genes involved in adhesion mechanisms that facilitate interactions and engraftment within the bone marrow environment.
This discovery provides compelling evidence that CD34-negative HSCs “could be more effective as a treatment option than current clinical use suggests,” says Al-Amoodi, the first author of the academic paper detailing these findings.
“Given how effectively CD34-negative cells integrate with the bone marrow niche,” she explains, “their use could prolong cell regeneration in the transplant recipient.”
Moreover, incorporating both CD34-positive and CD34-negative HSCs in transplantation procedures has the potential to enhance efficiency and cost-effectiveness, amplifying the therapeutic benefits of cord blood “since it would double the potential stem cell content,” she says.
REFERENCE
Al-Amoodi, A.S., Kai, J., Li, Y., Malki, J.S., Alghamdi, A., Al-Ghuneim, A., Saera-Vila, A., Habuchi, S. & Merzaban, J.S. α1, 3-Fucosylation treatment improves cord blood CD34 negative HSC navigation. iScience 27, 108882 (2024).| article.
JOURNAL
iScience
DOI
10.1016/j.isci.2024.108882
ARTICLE TITLE
α1,3-fucosylation treatment improves cord blood CD34 negative hematopoietic stem cell navigation
ARTICLE PUBLICATION DATE
16-Feb-2024

Leave a Reply