JULY 11, 2024
by University of North Carolina at Chapel Hill School of Medicine
Credit: Journal of Clinical Investigation (2024). DOI: 10.1172/JCI175616
Migraine is a chronic and debilitating neurological condition affecting women 3 to 4 more times than men. Despite an estimated 1.1 billion people being impacted by the condition, the physiological underpinnings of migraine remain mysterious, but are highly studied.
For the first time, researchers from the UNC School of Medicine’s Department of Cell Biology and Physiology have pieced together how a small protein called calcitonin gene-related peptide (CGRP) influences the lymphatic vascular system, contributing to the pain during migraine attacks. Their results were published in the Journal of Clinical Investigation.
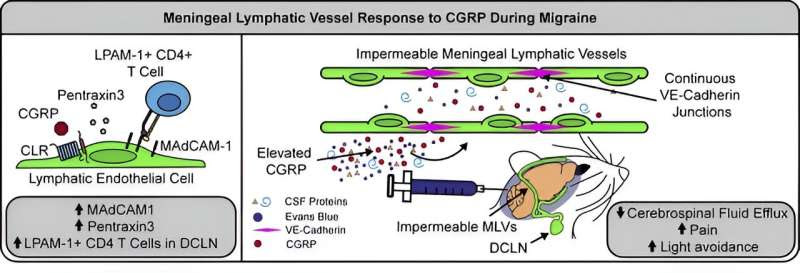
“Our study has highlighted the importance of the brain’s lymphatic system in the pathophysiology of migraine pain,” said Kathleen M. Caron, Ph.D., the Frederick L. Eldridge Distinguished Professor and chair of the Department of Cell Biology and Physiology and senior author on the study. “We found that migraine pain is influenced by altered interactions with immune cells and by CGRP preventing cerebrospinal fluid from draining out of the meningeal lymphatic vessels.”
CGRP, a small protein that is typically involved in pain transmission in neurons, is known to be elevated in the meninges, or the layers of tissues surrounding the brain, during migraine attacks. The team discovered that increases in CGRP levels also has a profound effect on the brain’s lymphatic vessels—a special system that facilitates the removal of cerebrospinal fluid and creates pathways for immune cells to patrol the protective covering of the brain.
To investigate how exactly CGRP influences the lymphatic system and contributes to migraine pain, the team of researchers performed a plethora of experiments in vitro and in vivo. Nate Nelson-Maney, a MD-Ph.D. student in the Caron lab and first author on the paper, spearheaded these experiments.
Using mouse models that were immune to the effects of CGRP, they first confirmed that they experienced less pain and spent more time in a brightly lit chamber compared to those that were vulnerable to CGRP. Bright light is a painful stimulus for people experiencing migraine, and the ability to measure similar behaviors in mice validates the translational impact of the study.
Using cell culture techniques, they assessed how a specialized protein is spatially arranged between the individual cells that line the lymphatic vessels. The protein, called VE-Cadherin, helps keep lymphatic endothelial cells stuck together and controls how much fluid, like cerebrospinal fluid, can squeeze between lymphatic endothelial cells and leave the vessels.
Researchers found that lymphatic endothelial cells that have been treated with CGRP rearrange their VE-Cadherin proteins so that they are aligned like a zipper on a jacket, keeping a tight seal. This arrangement prevents fluid from passing between cells, reducing the permeability of these cell layers.
They validated this finding in meningeal lymphatic tissue of mouse models treated with nitroglycerin-induced migraine. When CGRP and a traceable dye were injected into the meningeal lymphatic vessels, they observed a significant reduction in the amount of cerebrospinal fluid exiting from the skull.
Future studies are needed to reveal further information about the existing relationships between migraine, CGRP, and meningeal lymphatic vessels. The research team will work to understand how cerebrospinal fluid drainage through the meningeal lymphatic vessels contributes to migraine in humans through studies with and without the use of the latest FDA-approved CGRP-targeting medications, such as Nurtec, Emgality, Ajovy, etc.
Although CGRP has been identified as the main culprit behind migraine-inducing changes to the lymphatic system, researchers do not fully understand the pathophysiology of migraine triggers and pain. More research is needed to understand how meningeal lymphatic vasculature and the hormone-related life stages of women, such as puberty, pregnancy, and menopause, play a role in producing migraine.
“Since lymphatic dysfunction also exhibits a strong prevalence in women, it is tempting to speculate that neurological disorders like migraine could be governed by sex differences in the meningeal lymphatic vasculature,” said Caron, who is also a member of the UNC Lineberger Comprehensive Cancer Center. “If this were true, then new therapeutic strategies or drug targets that enhance meningeal lymphatic and glymphatic flow in women would be desirable.”
More information: Nathan P. Nelson-Maney et al, Meningeal lymphatic CGRP signaling governs pain via cerebrospinal fluid efflux and neuroinflammation in migraine models, Journal of Clinical Investigation (2024). DOI: 10.1172/JCI175616. www.jci.org/articles/view/175616
Journal information: Journal of Clinical Investigation

Leave a Reply