
By Dr. Priyom Bose, Ph.D.
Reviewed by Danielle Ellis, B.Sc.
Vitamin D3 is associated with multiple functions, including bone mineralization, regulation of cell growth, and immune and neuromuscular functions. The current article focuses on the role of vitamin D in hormonal balance and how it influences the development of many health issues, including infertility.

Image Credit: Photoroyalty/Shutterstock.com
Synthesis of vitamin D in humans
Vitamin D was first identified as a vitamin in the 20th century and is now recognized as a prohormone.1 There are different types of vitamin D, including fat-soluble secosteroids, i.e., vitamin D1-D5. In humans, vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are most important for biological functions.2 Vitamin D is mostly synthesized in the skin in the presence of sunlight, while some, particularly vitamin D2 and D3, are taken from food sources.
When human skin is exposed to sunlight, 7-dehydrocholesterol is transformed into D3; subsequently, it is converted to 25-hydroxyvitamin D (25(OH)D, also known as calcidiol or calcifediol, in the liver.3 The active form of vitamin D3, which is also known as calcitriol, 1α,25-dihydroxy vitamin D3, or 1,25-dihydroxycholecalciferol, is synthesized in the kidney in the presence of the enzyme 1α-hydroxylase. Vitamin D levels are determined by estimation of serum 25(OH)D.4
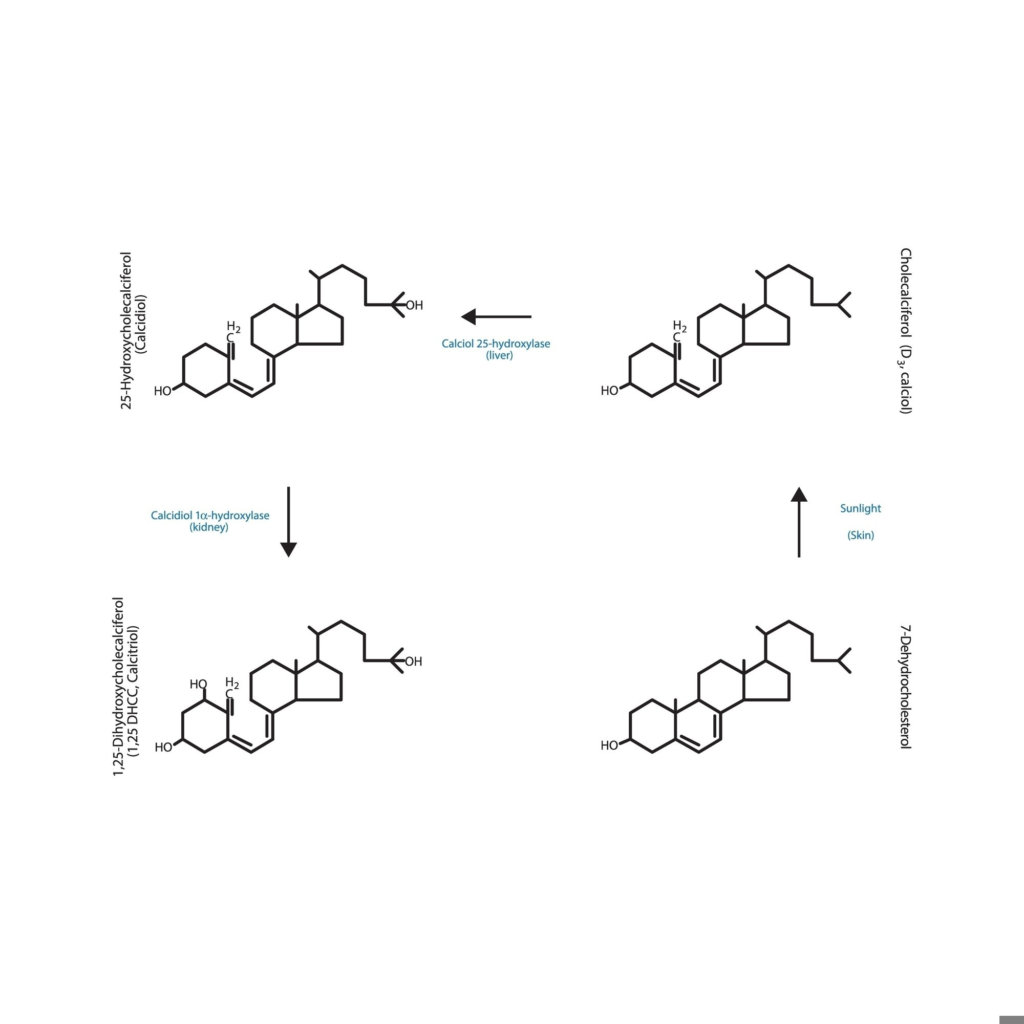
Diagram showing biosynthesis of active form of vitamin D – Calcitriol – via the kidneys and the liver – schematic molecular structure chemical illustration. Image Credit: Bass stock/Shutterstock.com
Vitamin D regulates calcium-phosphate metabolism and enhances calcium levels via multiple pathways.2 For instance, it is associated with the stimulation of calcium absorption in the intestine, its reabsorption in the renal tubules, and activation of the RANK/RANKL (receptor activator for nuclear factor κ B/its ligand) pathway in osteoclasts.5
Vitamin D and thyroid hormone
Thyroid glands synthesize hormones that regulate the functioning of physiological systems. The hypothalamus-pituitary-thyroid (HPT) axis regulates thyroid hormone synthesis through a feedback mechanism.6 When thyroid hormone levels decrease beyond a threshold point, the hypothalamus synthesizes thyrotropin-releasing hormone (TRH). Subsequently, TRH triggers thyrocytes that enhance thyroid hormone synthesis.
Vitamin D and parathyroid hormone (PTH) are involved in the regulation of calcium and bone formation. Vitamin D elevates calcium absorption from the small intestine, inhibits PTH, and decreases calcium excretion in the kidneys. This ultimately increases calcium concentration in the blood and promotes bone formation, growth, and maintenance.7
Autoimmune thyroid diseases, such as Hashimoto’s thyroiditis (hypothyroidism) and Graves’ disease (hyperthyroidism), are characterized by thyroid lymphocytic infiltration.8A meta-analysis observed a significant decrease in 25(OH)D levels in patients with Hashimoto’s thyroiditis. Similarly, another study revealed vitamin D deficiency is associated with the onset of Graves’ disease in older adults. Animal models of Graves’ disease and thyroiditis revealed the efficacy of vitamin D supplementation in alleviating these conditions.9
Vitamin D modulates the activity of many immune cells and is involved in immune cell regulation. Mechanistically, vitamin D receptor (VDR) and 1α-hydroxylase are expressed in immune cells, i.e., T and B lymphocytes, monocytes, dendritic cells, and neutrophils, which entails the production of calcitriol. Vitamin D enhances the production of anti-inflammatory cytokines (e.g., IL-4, IL-5, and IL-10) and inhibits proinflammatory cytokines (e.g., IL-6, IL-8, IL-9, IL-12, IFN-γ, and TNF-α) production. Multiple in vitro and in vivo studies have shown the positive effect of vitamin D in thyroid cancer treatment.10
Vitamin D and male hormones
25(OH)D levels regulate multiple enzymes involved in the production of steroid hormones, such as adrenal steroid hormones, sex hormones, and sex hormone signaling. Vitamin D metabolizes enzymes in the human testis and ejaculatory tract and is also associated with spermatozoa maturity.
Experimental findings have highlighted the possible role of vitamin D in male fertility through the synthesis of male reproductive hormones.11 A Mendelian Randomization analysis revealed the causal relationship between vitamin D deficiency and testosterone levels. This study linked a genetic decrease in 25(OH)D levels with lower testosterone levels. Another cross-sectional study supported this finding and highlighted a positive correlation between 25(OH)D levels and total/bioavailable testosterone levels. Men with lower serum 25(OH)D levels, particularly below 25 nmol/L, had a lower testosterone level.
These observations have drawn significant attention from the scientific community, which is seeking to understand better the potential impact of this vitamin on male reproductive function. Although more research is needed to understand how age, genetic variations, seasonal variations, and measurement timing influence testosterone levels, a recent study demonstrated that vitamin D supplementation enhances testosterone levels. Future research must also focus on the therapeutic potential of vitamin D in alleviating problems linked with male fertility.
Vitamin D and female hormones
Vitamin D influences estrogen and progesterone levels that impact menstrual regularity, menopause, fertility, and pregnancy.12 Animal-based experiments revealed that 25(OH)D deficiency reduced fertility rates, compromised mating behavior, and impaired neonatal growth.
Decreased maternal vitamin D levels have been associated with poor maternal and fetal outcomes, including gestational diabetes mellitus, low birth weight, preeclampsia, and small for gestational age. Many women experience polycystic ovary syndrome (PCOS), a heterogeneous endocrine disorder that causes female infertility and is associated with hyperandrogenism. Multiple studies have observed serum vitamin D deficiency in patients with PCOS. Mechanistically, vitamin D deficiency influences insulin secretion and insulin resistance, which could induce PCOS.13
Research has established a link between vitamin D and reproduction hormone biosynthesis. 14 An inverse correlation between vitamin D levels and androstenedione and anti-Müllerian hormone, as well as follicle-stimulating hormone (FSH)/luteinizing hormone (LH), has also been found. One recent study recommended women with PCOS consume 400 IU of vitamin D supplementation and 1000 mg of calcium daily for three months to improve fertility and other PCOS symptoms.
References
Institute of Medicine (US) Committee to Review Dietary Reference Intakes for Vitamin D and Calcium; Ross AC, Taylor CL, Yaktine AL, et al., editors. Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): National Academies Press (US); 2011. 3, Overview of Vitamin D. Available from: https://www.ncbi.nlm.nih.gov/books/NBK56061/
Voltan G, Cannito M, Ferrarese M, Ceccato F, Camozzi V. Vitamin D: An Overview of Gene Regulation, Ranging from Metabolism to Genomic Effects. Genes. 2023; 14(9):1691. https://doi.org/10.3390/genes14091691
Bikle DD. Vitamin D metabolism, mechanism of action, and clinical applications. Chem Biol. 2014;21(3):319-329. doi:10.1016/j.chembiol.2013.12.016 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3968073/
Han, F., Wang, Y., Li, J., Li, Z., Mu, D., He, L., & Zhang, J. (2023). Wei sheng yan jiu = Journal of hygiene research, 52(1), 129–135. https://doi.org/10.19813/j.cnki.weishengyanjiu.2023.01.022
Chacar FC, Kogika MM, Zafalon RVA, Brunetto MA. Vitamin D Metabolism and Its Role in Mineral and Bone Disorders in Chronic Kidney Disease in Humans, Dogs and Cats. Metabolites. 2020; 10(12):499. https://doi.org/10.3390/metabo10120499
Feldt-Rasmussen, U., Effraimidis, G., & Klose, M. (2021). The hypothalamus-pituitary-thyroid (HPT)-axis and its role in physiology and pathophysiology of other hypothalamus-pituitary functions. Molecular and Cellular Endocrinology, 525, 111173. https://doi.org/10.1016/j.mce.2021.111173
Khundmiri SJ, Murray RD, Lederer E. PTH and Vitamin D. Compr Physiol. 2016;6(2):561-601.. doi:10.1002/cphy.c140071
Vieira IH, Rodrigues D, Paiva I. Vitamin D and Autoimmune Thyroid Disease-Cause, Consequence, or a Vicious Cycle?. Nutrients. 2020;12(9):2791.. doi:10.3390/nu12092791
Babić Leko M, Jureško I, Rozić I, Pleić N, Gunjača I, Zemunik T. Vitamin D and the Thyroid: A Critical Review of the Current Evidence. Int J Mol Sci. 2023;24(4):3586.. doi:10.3390/ijms24043586
Gallo D, Baci D, Kustrimovic N, et al. How Does Vitamin D Affect Immune Cells Crosstalk in Autoimmune Diseases?. Int J Mol Sci. 2023;24(5):4689. doi:10.3390/ijms24054689
de Angelis C, Galdiero M, Pivonello C, et al. The role of vitamin D in male fertility: A focus on the testis. Rev Endocr Metab Disord. 2017;18(3):285-305. doi:10.1007/s11154-017-9425-0
Kolcsár M, Berecki B, Gáll Z. Relationship between Serum 25-Hydroxyvitamin D Levels and Hormonal Status in Infertile Women: A Retrospective Study. Diagnostics (Basel). 2023;13(19):3024. doi:10.3390/diagnostics13193024
Mohan A, Haider R, Fakhor H. et al. Vitamin D and polycystic ovary syndrome (PCOS): a review. Ann Med Surg (Lond). 2023;85(7):3506-3511. doi: 10.1097/MS9.0000000000000879. https://pubmed.ncbi.nlm.nih.gov/37427232/
Chu C, Tsuprykov O, Chen X, Elitok S, Krämer BK, Hocher B. Relationship Between Vitamin D and Hormones Important for Human Fertility in Reproductive-Aged Women. Front Endocrinol (Lausanne). 2021;12:666687. doi: 10.3389/fendo.2021.666687. https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.666687/full

Leave a Reply