August 13, 2024
by Matt Shipman, North Carolina State University
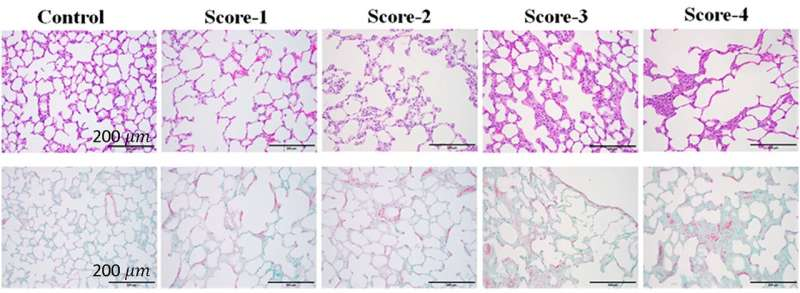
Examples of histology slides corresponding to modified Ashcroft scores 0–4, for H&E (top) and Masson’s trichrome (bottom) staining. Viewed at 100 × total magnification. Scale bar = 200 microns. Credit: Scientific Reports (2024). DOI: 10.1038/s41598-024-66390-6
Researchers have established a suite of parameters that can be determined using ultrasound to quantitatively measure different physical characteristics of the lung. The researchers also demonstrated that the parameters can be used to accurately diagnose and assess the severity of lung diseases in an animal model.
The paper, “Lung quantitative ultrasound to stage and monitor interstitial lung diseases,” is published open access in the journal Scientific Reports.
“Diseases can affect lungs in many different ways,” says Marie Muller, co-senior author of a paper on the work and an associate professor of mechanical and aerospace engineering at North Carolina State University. “They can change the microstructure of the lung, the elasticity of the lung tissue, the type and amount of fluid in the lungs, and so on. Each of these changes can be measured using ultrasound. Our goal with this work was to establish clear parameters for these lung characteristics and determine which combination of parameters is associated with different lung diseases.”
“To be clear, we’re talking about numeric measurements for each parameter,” says Muller, who is also on faculty in the Joint Biomedical Engineering Department at NC State and the University of North Carolina at Chapel Hill.
“So, if there are three parameters associated with a disease, we’d have three numbers—one for each parameter. We can then use a mathematical formula that combines those three numbers to create a biomarker score. That score not only tells us whether a specific health problem is present, but how severe the problem is.”
The researchers began by generating parameters for measuring a wide variety of lung characteristics, such as the density of alveoli or the amount of fluid in the lungs. The researchers also adapted existing ultrasound parameters used in other organs for use on lung tissue. Altogether, this resulted in a total of 60 parameters.
The researchers then measured all 60 parameters in the lungs of rats that were healthy or had various stages of fibrosis or edema. Fibrosis is scarring of the lung tissue. Edema refers to fluid build-up in the lung.
“We then used statistical methods to identify which combinations of parameters were both associated with a given health condition and sensitive enough to measure the severity of a health problem,” Muller says.
Through this process, the researchers found that only five of the parameters were necessary for assessing fibrosis and edema: three for fibrosis and two for edema.
“One of the challenges with many diagnostic tools is that there is often a trade-off between sensitivity and specificity,” Muller says. “A highly sensitive test may virtually guarantee that you detect a problem, but it also usually means that there can be a lot of false positives. On the other hand, a highly specific test will almost never give you a false positive, but it may also miss quite a few health problems it is supposed to detect, or not be able to assess the severity of a specific disease.”
“We’re excited about this new diagnostic tool because it is both highly sensitive and highly specific,” Muller says. “And we’re able to have that combination of specificity and sensitivity because we are measuring multiple parameters.”
One way they were able to assess the sensitivity of the new tool is by making use of fibrosis treatments. As rats who had fibrosis received treatment, the new diagnostic tool was able to measure improvements in the rats’ lung tissue.
The researchers have developed data processing software that can be used in conjunction with existing ultrasound hardware to determine the numbers for each parameter measurement, as well as establishing the biomarker scores for edema and fibrosis.
“We’ve established that this works well in a rat model,” Muller says. “Next steps involve computational simulations, in vitro testing, and animal model testing to establish that this technique can work in cases where the ultrasound has to penetrate a much thicker chest wall. If that goes well, we’ll pursue clinical trials.
“Also, because we have established 60 parameters—which is a lot—we’re optimistic that this technique can be used in the future to identify diagnostic biomarkers for a range of other lung conditions.”
More information: Azadeh Dashti et al, Lung quantitative ultrasound to stage and monitor interstitial lung diseases, Scientific Reports (2024). DOI: 10.1038/s41598-024-66390-6
Journal information: Scientific Reports
Provided by North Carolina State University

Leave a Reply