September 3, 2024
by Aarhus University
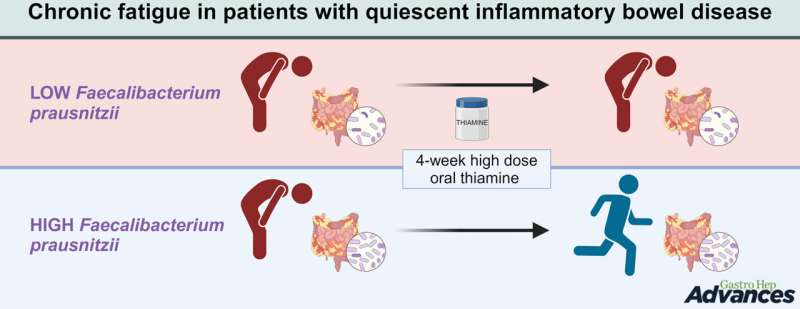
Graphical abstract. Credit: Gastro Hep Advances (2024). DOI: 10.1016/j.gastha.2024.08.012
Fatigue is a common and often debilitating companion for people with inflammatory bowel conditions. Now, a new Danish study provides insight into why vitamin B1—also known as thiamine—helps some patients regain their energy, while others do not experience the same effect. The findings are published in the journal Gastro Hep Advances.
The study shows, among other things, that patients’ response to vitamin B1 depends on gut bacteria, with researchers focusing particularly on a specific “good bug” that seems to play a crucial role.
“We know that about half of the fatigued patients benefit from treatment with vitamin B1, but we haven’t been able to find anything that distinguishes those who had an effect from those who did not. Now we know that it’s especially the bacterium Faecalibacterium prausnitzii (FP) that is the key,” says Professor and Consultant Christian Lodberg Hvas, who is the lead author of the study.
Surprising findings
FP is a bacterium that many studies have identified as having beneficial properties or at least being frequently found in people with a healthy gut.
The researchers were surprised to find that the presence of a single key bacterium determines whether patients with chronic fatigue experience a good effect from thiamine treatment.
“We thought we were looking for a ‘fatigue microbiome,’ a composition of gut bacteria that is particularly seen in patients with chronic fatigue. But we didn’t find that. Instead, we found that the microbiome of the fatigued largely resembles the microbiome of those who are not fatigued,” explains Lodberg Hvas.
Still a mystery
The study involved 40 patients with inflammatory bowel disease and chronic fatigue. Each patient received both vitamin B1 and a placebo in two periods of four weeks with a break in between. This allowed the researchers to see if the vitamin treatment had an effect on fatigue.
At the same time, the researchers examined the patients’ gut bacteria to see if there was a correlation between specific bacteria and the effect of the treatment.
Although the researchers found a clear connection between FP and the patients’ response to the treatment, it remains a mystery why this is the case.
“The bacterium is largely present in people with good health and only present in low numbers in people with chronic diseases. We don’t know if it’s just a marker for health or if it’s part of the reason why healthy people are indeed healthy,” explains Lodberg Hvas.
“But the more studies that point to a beneficial effect of FP, the more it suggests that the bacterium is involved as a cause of health and not just as a bystander,” he adds.
A cure for many with unexplained fatigue
For some patients, fatigue can be explained by a lack of iron, vitamin D, or low thyroid function. These are all conditions that are easy to treat. But a large group of patients with inflammatory bowel disease remains with unexplained fatigue.
“We really want to help them, and although we don’t have an explanation, we now have a cure—for those who have many FP in their gut,” says Lodberg Hvas. “Therefore, we now recommend high-dose vitamin B1 treatment to all our patients where we don’t find any obvious explanation for chronic fatigue. We know that it only works for half, but it’s still a good chance, and a month’s treatment is cheap,” he adds.
The clear recommendation also comes because the treatment has proven to be completely free of side effects.
“However, one must accept that thiamine smells and tastes peculiar—so your hands, urine, and sweat will smell like vitamin pills with the very high dose you’re taking,” says Lodberg Hvas.
More information: Sandra Bermúdez-Sánchez et al, Thiamine-reduced fatigue in quiescent inflammatory bowel disease is linked to Faecalibacterium prausnitzii abundance, Gastro Hep Advances (2024). DOI: 10.1016/j.gastha.2024.08.012
Provided by Aarhus University

Leave a Reply