07 September 2024
ByCarly Cassella
(Derek Berwin/Getty Images)
The human papillomavirus (HPV) is responsible for the vast majority of cervical cancer cases, but this isn’t a sexually transmitted infection that just one half of the population needs to worry about.
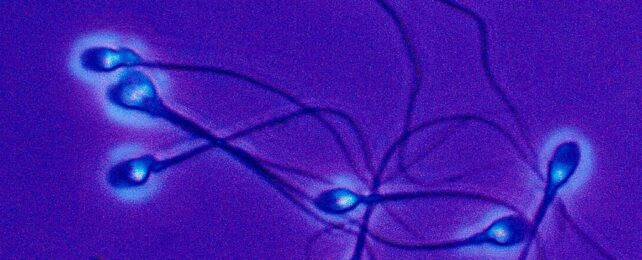
Researchers from Argentina have found strains of HPV which put people at high risk of cancer are associated with a greater percentage of dead sperm.
In semen samples from those with high-risk strains, scientists noticed a lower count of white blood cells and an elevation of reactive oxygen species, which can damage sperm and alter DNA.
Samples from those with low-risk HPV did not show the same correlations.
The findings are only based on semen samples from 205 adult males, however they align with previous findings linking HPV to lower sperm count and reduced motility and viability, indicating an insidious impact on male fertility.
“Here we show that genital HPV infection is very prevalent in men, with variable effects on semen inflammation and sperm quality according to the infecting viral genotype,” explains infection microbiologist Virginia Rivero from the National University of Córdoba in Argentina.
“Specifically, infections caused by high-risk HPV genotypes appear to have more negative effects on male fertility and the immune system’s ability to clear the infection.”
Currently approved clinical tests for HPV look for the virus in cervical screens. This is probably one reason why today, the full range of effects that HPV can have on male bodies is relatively under-explored.
HPV is known to cause cancer in the penis, anus, mouth, and throat of male patients. Its DNA can be detected at these sites with the right diagnostic tools. But historically, this infection has been ‘feminized’ in a way that some researchers argue is dangerous for public health.
When the HPV vaccine first became available in 2006, it was only approved in the US for young female patients. It took three years before the US Food and Drug Administration also approved the medicine for young male patients, and another two years before the Centers for Disease Control and Prevention’s Advisory Committee on Immunization Practices seconded that advice.
As of 2022, the World Health Organization recommends that the HPV vaccine is included in routine childhood vaccinations for males and females. Yet even still, the “primary target of vaccination is girls aged 9 to 14”. Boys are only considered “secondary targets” where “feasible and affordable”.
Only about one third of the 107 nations with vaccination programs for HPV have included boys in their roll-out. In 2019, about 4 percent of boys globally had received the full course of the vaccine compared to 15 percent of girls.
In the US specifically, HPV vaccination rates among teen boys are slightly lower than for girls – at 61 percent versus 65 percent in 2022.
In Australia, which has the most successful HPV vaccination program in the world, coverage rates in 2023 were as high as 85.9 percent for females and 83.4 percent for males.
“A lot of men object to the HPV vaccine and will say, ‘Why should I get this when it is for girls?'” explains public health scientist Nosayaba Osazuwa-Peters from Duke University, who led a recent study on disparities in HPV vaccine uptake.
The new research from Argentina offers a new reason.
The study analyzed the sperm of 205 adult male volunteers who had not been vaccinated against HPV but who had presented at a urology and male reproductive health clinic.
Their semen was tested for the presence or absence of HPV and other STIs. Nearly 20 percent tested positive for HPV, and 20 men had strains that were deemed ‘high risk’.
Compared to 43 men with no HPV infections, those with high-risk HPV showed some disturbing changes to their semen that weren’t picked up by WHO-recommended analysis methods.
Using a more sensitive test, Rivero and colleagues found men with high-risk HPV showed increased sperm death, possibly due to oxidative stress and a weakened local immune response.
“Our study raises important questions about how high-risk-HPV affects sperm DNA quality and what implications it has for reproduction and offspring health,” says Rivero.
Cervical cancer cases have dropped – by almost 90 percent in the UK – thanks to the HPV vaccine, but throat and penile cancers associated with HPV are on the rise.
In 2021, two public health scientists from Uppsala University in Sweden argued that vaccinating everyone against HPV, regardless of their sex, “is the only way” to eradicate this all too common infection and its long-term health consequences.
If HPV continues to be primarily regarded as a ‘woman’s problem’, this virus may forever wreak havoc on both male and female fertility.
The study was published in Frontiers in Cellular and Infection Microbiology.

Leave a Reply