
ofessor at Harvard Medical School, but in many ways, Dr. Victor Gurewich is an outsider.
His research is funded by a small family foundation, and he hasn’t tried for a federal grant in decades. He’s a primary care doctor whose work tramples on the terrain of cardiologists and neurologists.
So it’s perhaps not surprising that, more than 20 years after figuring out a combination therapy that he believes is a safer, more effective way to treat heart attacks and strokes, he’s had little success getting anyone to listen.
Now at age 88, Gurewich is still trying to convince his medical peers that he’s right, and a tiny company he started in 2006 is about to launch a clinical trial in Europe that he hopes will prove it.
“I’m stubborn. I don’t give up,” he said during an interview in the modest Cambridge, Mass., offices of Thrombolytic Science International, where the built-in bookshelves are lined with his lab notebooks, meticulously hand-labeled and dating back to 1963.
His long struggle to be heard offers insight into how promising research ideas sometimes fail to take hold — even in the face of favorable evidence — said Gregory del Zoppo, a University of Washington expert on stroke treatment who saw enough promise in Gurewich’s data to join the company’s clinical advisory board.
Several heart and stroke specialists told STAT they knew nothing about Gurewich’s work, or else they dismissed his experimental therapy as outmoded.
Others said he should keep plugging away to see whether his drug combination can be shown safe and effective in patients. “It’s a nifty idea. Who knows, maybe it’s a great idea,” said Stephan A. Mayer, chairman of neurology for the Henry Ford Health System in Detroit.
Twenty-three years ago, Gurewich published a clinical trial in heart attack patients, showing his idea of combining two medications to break up blood clots had merit. But the company that ran the study was sold, and the buyer shut down its cardiology division. Since then, as he’s labored to get financial backing, another drug became the standard of care in stroke, while clot-busting drugs were abandoned as a treatment for heart attacks.
“It’s just a remarkable story,” said Annalisa Jenkins, a British doctor and biotech executive who serves on the TSI board. She signed on, she said, because she believes in the science and wants to help the company succeed. She also believes in Gurewich.
“I just love him to bits,” she said. “His whole life has been unraveling this [medical] pathway. … He’s not in it for the commercial success. It’s part of his legacy.”
End up in a hospital today with a heart attack, and you’re likely to be rushed in for an emergency angioplasty. An interventional cardiologist will thread a catheter through your arteries until reaching the site of the blockage in your heart that caused the attack. By inflating a tiny balloon, the doctor will push the clot out of the way, allowing blood to flow through again.
The faster the better, but many patients get to the hospital after the first few hours, when most of the damage happens.
If, instead, you have a type of stroke caused by a similar blockage in the blood vessels of the brain, speed is also essential. A doctor may perform surgery to break up clots in larger vessels, but that procedure is still too risky in smaller ones. In those cases, you might receive a drug called tissue plasminogen activator, or tPA. If given within 4 1/2 hours after a stroke begins, the medication can help dissolve the clot, restore blood flow, and reduce brain damage. But tPA can also cause seizures and fatal brain bleeds, which makes some doctors reluctant to use it.
Gurewich believes his treatment approach could solve both problems: The medications could quickly open up blocked vessels, providing stroke patients effective treatment at lower risk, and giving heart attack patients more time to get an angioplasty or — in areas or countries where the procedure is too expensive or readily available — an effective alternative.
He has the type of scientific data that usually convinces medical minds to run a large clinical trial in the hopes of winning FDA approval of their drug. But Gurewich often feels like he’s tilting at windmills.
“It’s all pretty obvious,” Gurewich said of his approach, because that’s how clots are naturally dissolved in the body. “What’s not so obvious is why it’s ignored.”
“It’s a nifty idea. Who knows, maybe it’s a great idea.”
STEPHAN A. MAYER, CHAIRMAN OF NEUROLOGY FOR THE HENRY FORD HEALTH SYSTEM
The story begins in 1980, when Gurewich discovered a precursor to an enzyme, called urokinase plasminogen activator.
We can survive cuts and bruises without bleeding to death because of our blood’s ability to form clots. The body also has a compensatory clot-busting system to dissolve clots that form inside blood vessels: tPA is part of that natural system; urokinase is, too.
Urokinase was already being used as a clot-buster in people with clots in their lungs, but it sometimes led to brain bleeds, because it didn’t target just the clot.
Gurewich’s urokinase precursor was less likely to lead to brain bleeds, because it was clot-specific, but when he published that finding, it had no impact.
Although he hadn’t yet met Gurewich, del Zoppo was a big fan of urokinase in those days, and of the idea that drugs could be used within a few hours of a stroke to help the brain recover. He helped lead clinical trials of tPA, which proved more popular than urokinase, in part because it could be delivered more easily. Urokinase was injected into an artery in the thigh, while the doctor watched for the clot to dissolve. With tPA, doctors simply had to add a standard dose to a patient’s IV drip “and hope for the best,” said Mayer, of Henry Ford.
Although tPA failed at least half the time, and could have devastating side effects, tPA became the standard of care, with the entire emergency care system redesigned to make sure stroke patients could receive it quickly enough, del Zoppo said.
Gurewich was still convinced he had a better approach, so he went back to his lab, hoping to generate results that couldn’t be ignored.
Gurewich has always loved the satisfaction of research.
“As a boy, I was always taking things apart,” he said, laughing at his limited success at putting mechanical toys and other things back together. “It is fun to think about how something works.”
He was 6 when his family fled Hitler’s Berlin. Gurewich was raised mostly in London and New York, where several German Nobel laureates were regular guests of his doctor father’s.
He came to Boston in the late 1950s for medical school at Harvard, where a mentor encouraged him to pursue his curiosity and take up research projects on the side. It was an unusual activity for a practicing doctor at the time. Ever since, he’s balanced a half-time medical practice — he still sees patients four half-days a week, at Mount Auburn Hospital in Cambridge — and research.
“I’m interested in blood vessels,” he said. People think of heart disease as occurring in the heart, but, really, most of the action happens in the coronary blood vessels, he said.
In the early 1980s, when his research was federally funded, Gurewich figured out that urokinase and tPA functioned as a team in the body. But he didn’t understand how the process worked.
One night, he woke up thinking about the problem. “It killed the rest of the night,” he said. But by first light, he had an idea: What if tPA worked like the starter motor that turns on a car, and urokinase was the gasoline that ran it?
Back in his lab, he proved at least experimentally that he was right. When a clot forms, tPA in the bloodstream is quickly recruited to the site to begin dissolving it. But too much of a clot-buster could lead to bleeds, so once the process is sparked, the body rapidly clears out tPA. Urokinase comes along, carried on the surface of platelets and certain white blood cells, to finish the job.
The mistake that everyone, including him, had made, Gurewich realized, was that they had treated patients with just one drug or the other. They needed both.
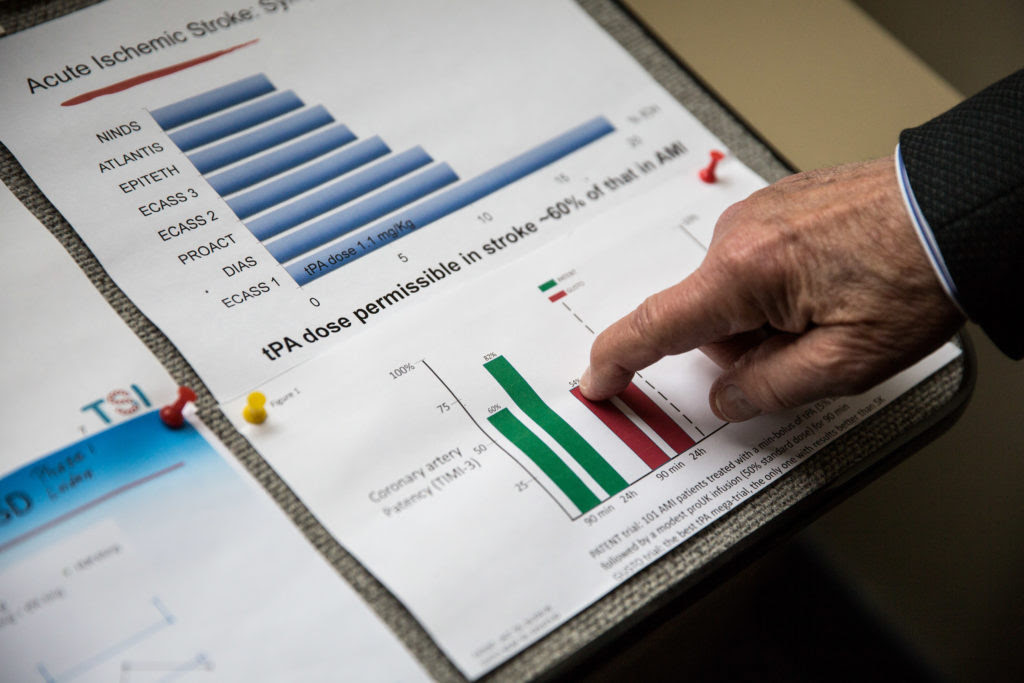
One early study had found that tPA reopens blockages in about 45 percent of heart attack patients, but also leads to death in about 6 percent of them. In a 1995 clinical trial, Gurewich showed that the combination of tPA plus his urokinase precursor, called pro-UK, could open 77 percent of blockages. One out of his 101 patients died in the hospital — a death rate of just 1 percent. The trial was not a gold-standard randomized trial, however; it didn’t compare tPA head to head with the combination therapy.
Gurewich is modest about his role in this discovery. “We didn’t invent anything,” he said. “We just figured out how it works, which is sometimes all it takes.”
But it would take more than that.
A European pharmaceutical company had licensed Gurewich’s form of pro-UK and funded the 1995 trial, after seeing his earlier, promising results. But the company was sold to another, which had different priorities and gave Gurewich back the license.
He tried to find another company to support his research, but by the late 1990s and early 2000s, the field was focused on getting tPA into patients fast enough.
Other people were tinkering with different drugs in this class, called thrombolytics. Some of these drugs fared well in mid-sized trials, but none made it all the way to market.
Gurewich refused to give up. He set out to improve pro-UK’s main weakness: In the body, it quickly converted to urokinase and caused bleeding.
He started TSI in 2006 to fund the work, and eventually, he came up with a modified version of pro-UK that converted to urokinase more slowly, and therefore was safer.
By that point, though, the mixed results from tPA had so discredited the whole idea of such thrombolytic drugs in treating heart attacks that cardiologists dismiss the entire drug category out of hand. “We’ve moved away from thrombolytics for a long time now,” Robert Yeh, an interventional cardiologist at Beth Israel Deaconess Medical Center and Harvard Medical School, said via email. Heart attacks are instead treated with angioplasty.
tPA is still considered valuable for stroke patients, though as many as 30 percent of patients who might benefit don’t receive it — at least in part, according to a recent New York Times story, because their doctors are dubious of its benefits.
Gurewich feels strongly that giving tPA by itself is a bad idea. “It’s quite remarkable that they’re still using tPA alone,” he said. “It’s a bit of a scandal. More than a bit.”
Now, Gurewich and TSI’s staff of one are poised to start a clinical trial in 100 stroke patients in the Netherlands in June, with the $1 million to $2 million cost picked up by the same private foundation that has kept the company going all these years. If Jenkins can help the company raise $5 million to 10 million in the next few months, it will launch a second trial in heart attack patients in London.
Gurewich’s hope is that the clinical trials will finally prove to the world that his one-two punch can safely knock out clots in the heart and the brain. A successful pilot trial should be enough to convince a major pharmaceutical company to invest in the idea, buy up TSI, and conduct the larger, more expensive trials that would be needed to bring it to market, Jenkins said.
Although stroke specialists are moving away from tPA now, in favor of surgery, Dr. David Liebeskind, a professor of neurology at the University of California, Los Angeles, said the right drug could still catch the field’s attention. To displace tPA, a new drug would have to be at least as safe, effective, and easy to use, he said. Cheaper would help, too. The price of tPA has recently rocketed up from about $2,000 to $8,700 per vial, he said.
Gurewich remains perennially optimistic.
“Now there’s a hope we really will get this on the market and used,” he said.
