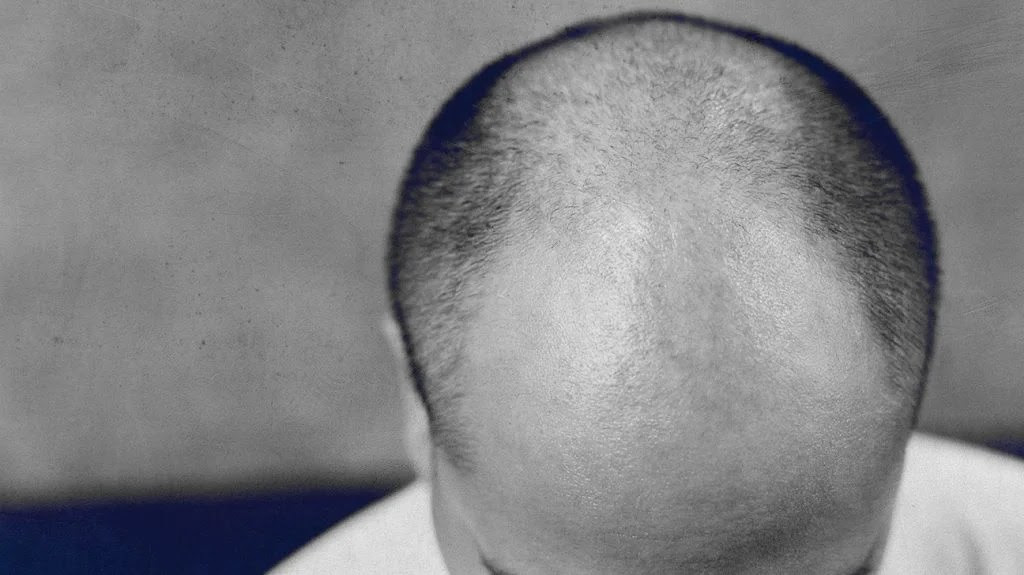
New research reviews potential links between male sex hormones and susceptibility to severe COVID-19. Rattanakun Thongbun/EyeEm
- The European Society of Endocrinology updated its advice about the interplay between hormones, metabolism, and COVID-19.
- The statement reviews evidence of the additional risks for people with diabetes, obesity, low vitamin D levels, and pituitary, adrenal, and thyroid disorders.
- It also explores why males are more susceptible than females to severe COVID-19 and discusses the treatment potential of drugs that block male sex hormones.
- Finally, the statement provides reassurance that COVID-19 vaccination is safe for people with hormone-related (endocrine) disorders.
Early in the pandemic, it became clear that males are more susceptible than females to severe COVID-19 and have a higher risk of death from the disease.
Among the proposed reasons are higher rates of smoking among males and a greater reluctance to wear a mask, but there may be a more fundamental, biological explanation.
SARS-CoV-2, which is the virus that causes COVID-19, exploits two membrane receptors called ACE2 and TMPRSS2 to break into its host cells.
Research suggests that androgens — that is, male sex hormones — increase the production of these receptors in the cells that line the airways of the lungs, which may make it easier for the virus to infect lung tissue in males.
Other lines of evidence that implicate male sex hormones include the observation that male pattern baldness, which is caused by high circulating levels of dihydrotestosterone (DHT), is associated with severe COVID-19 in males.
Intriguingly, clinical trials suggest that drugs for treating prostate conditions and male hair loss, which reduce the production of DHT or block the hormone’s receptors, may speed the recovery of people with COVID-19.
Leading endocrinologists from Spain, Turkey, and Italy have reviewed the latest evidence on male hormones and several other hormone-related risk factors for COVID-19 in a position statement for the European Society of Endocrinology.
The statement updates a previous statement that the society published in March 2020, early in the pandemic.
The authors write that physicians should exercise caution when prescribing testosterone — in particular, androgen replacement therapy for male hypogonadism in older patients.
They also review the evidence and issue advice for a range of other endocrine conditions, including vitamin D insufficiency, diabetes, obesity, adrenal insufficiency, and issues related to the pituitary and thyroid glands.
Low levels of vitamin D
“We need to be aware of the endocrine consequences of COVID-19 for patients with a known endocrine condition, such as diabetes, obesity, or adrenal insufficiency, but also for people without a known condition,” says first author Manuel Puig-Domingo, M.D., Ph.D., from the Universitat Autònoma de Barcelona in Spain.
“Vitamin D insufficiency, for example, is very common, and the knowledge that this condition has emerged frequently in the hospitalized COVID-19 population and may negatively impact outcomes should not be taken lightly.”
Despite its name, vitamin D is not a vitamin, but a hormone precursor.
After adjusting for known risk factors, low levels of the vitamin are more prevalent in people hospitalized with COVID-19 than in the general population.
Some studies have also found that low vitamin D levels are associated with more severe disease and mortality.
The authors recommend that healthcare professionals ensure that their patients have adequate vitamin D levels — in particular, older adults with diabetes or obesity.
They observe that home confinement during lockdowns, especially for older adults, may have contributed to worsening levels of vitamin D deficiency in some countries.
Worse outcomes for people with diabetes
The endocrinologists note that a large body of published evidence suggests that diabetes, poor management of blood glucose, and obesity are strong risk factors for worse outcomes and mortality in COVID-19.
“Active vigilance and testing in outpatient endocrine clinics, as well as early hospitalization for COVID-19 is recommended,” they write.
They add that treatment with metformin for type 2 diabetes and statins for high cholesterol are associated with less severe disease and lower risk of death, so these should not be stopped upon admission to the hospital.
Beta cells in the pancreas, which produce insulin, may be particularly vulnerable to damage by the virus because they express an abundance of ACE2 receptors.
This may partly explain new cases of diabetes following severe COVID-19.
The experts say:
“Mortality in type 1 or type 2 diabetes has consistently increased during the year of pandemic — and evidence is emerging that a bidirectional relationship between diabetes and COVID-19 may exist, both in terms of worsening existing conditions and new onset of diabetes.”
Lockdown may contribute to weight gain
Alongside diabetes, obesity has emerged as a major risk factor for COVID-19.
The authors write in their paper:
“Weight management, blood pressure, and blood glucose control have always been important to improve cardiometabolic health and prevent severe health consequences in obesity, but the risk of severe COVID-19 is now another important reason to focus on these issues.”
They caution that lockdown measures, by influencing diet, levels of physical activity, stress, and sleep, may lead to weight gain.
“Thus, people with obesity should be encouraged to increase physical activity and gain healthy eating habits, develop strategies to reduce stress and optimize sleep during pandemic,” they write.
Direct damage to endocrine glands
In addition to the effect of SARS-CoV-2 on the pancreas, they write that there is evidence that the virus may directly damage the adrenal, pituitary, and thyroid glands.
They review the latest evidence and provide clinical advice for the treatment of conditions related to each of these endocrine organs.
Finally, the endocrinologists emphasize that clinical trials of COVID-19 vaccines demonstrated similar efficacy and safety in patients with stable diabetes and obesity, compared with healthy subjects.
They recommend that vaccination should not be handled differently in patients with stable endocrine diseases such as autoimmune thyroiditis, Graves’ disease, Addison disease, pituitary adenomas, type 1 and 2 diabetes, and obesity.
However, they note that the treatment of patients with conditions such as Addison disease, in which the adrenal glands do not produce enough hormones, may require adjustment to address potential side effects of vaccines, such as fever.

Leave a Reply