By Carissa Wong
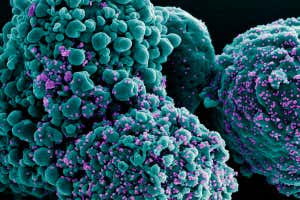
A coloured scanning electron micrograph of a cell (green) infected with the omicron variant of the coronavirus (purple)
NIAID / NATIONAL INSTITUTES OF HEALTH / SCIENCE PHOTO LIBRARY
Being infected with the omicron variant of the coronavirus may give some protection against flu.
Martin Michaelis at the University of Kent in the UK and his colleagues collected bronchial cells from a person with emphysema, a condition where the lungs’ air sacs are damaged, but the bronchi airways are unaffected.
The cells were extracted as part of a standard diagnostic or treatment procedure. With the bronchi being unaffected by emphysema, the results are expected to apply to people without the condition, according to Michaelis.
In a laboratory study, the bronchial cells were infected with the delta variant of the coronavirus, the BA.1 omicron subvariant – the original omicron variant – or the BA.5 omicron subvariant, which is currently dominant.
As a control, the researchers treated some cells with a saline solution that didn’t contain any coronavirus variant.
After two days, the team exposed the SARS-CoV-2-infected cells and the control cells to the H1N1 strain of influenza virus. H1N1 was responsible for the global swine flu outbreak in 2009-10. It is now one of the seasonal flu viruses that circulate every winter.
One day later, the researchers measured the H1N1 levels in all the cells. In the control cells and those infected with the delta variant, H1N1 levels increased by roughly 10,000-fold. This is compared with no increase in the cells containing either omicron subvariant.
The team also found that the cells containing the omicron subvariants produced a protective immune response called the interferon response, which is known to reduce the replication of flu viruses. Among the control cells and those infected with the delta variant, this response was much lower and insufficient to suppress H1N1 replication.
The findings may be reflective of SARS-CoV-2 and flu infection rates over the pandemic.
“Following the lifting of restrictions in July 2021 in England, we saw a delta wave accompanied by an increase in influenza-like illnesses, those diagnosed as the flu and those which seemed to be the flu,” says Michaelis. “But then, since omicron BA.1 became dominant, influenza-like illnesses dropped and have stayed low.”
However, these patterns could be due to other factors, such as people being more careful to avoid infections during winter, he says.
Understanding how different covid-19 variants trigger varying immune responses may help researchers more quickly understand the potential impact of new variants.
“Apart from out of curiousity, such findings can help to reveal how covid variants differ and could help us to understand and predict how any new variants that appear might behave,” says Michaelis.
The work doesn’t suggest people should purposely catch covid-19 to avoid flu, the researchers have stressed.
“We, of course, don’t advise people to purposely get infected with covid-19 to protect against influenza. With SARS-CoV-2 infection, there’s always a chance you could die,” says Michaelis.
If you are admitted to hospital with both covid-19 and flu, you are more likely to become critically ill and die, says Kenneth Baillie at the University of Edinburgh, UK.
What’s more, the results are based on a laboratory model, which may not translate well to people, says Michaelis.
Nevertheless, such work is of interest to virologists and supports decades of research that has found infecting cells with one virus makes it harder to infect them with another, says Baillie.
Reference: bioRxiv

Leave a Reply