by Justin Jackson, Medical Xpress
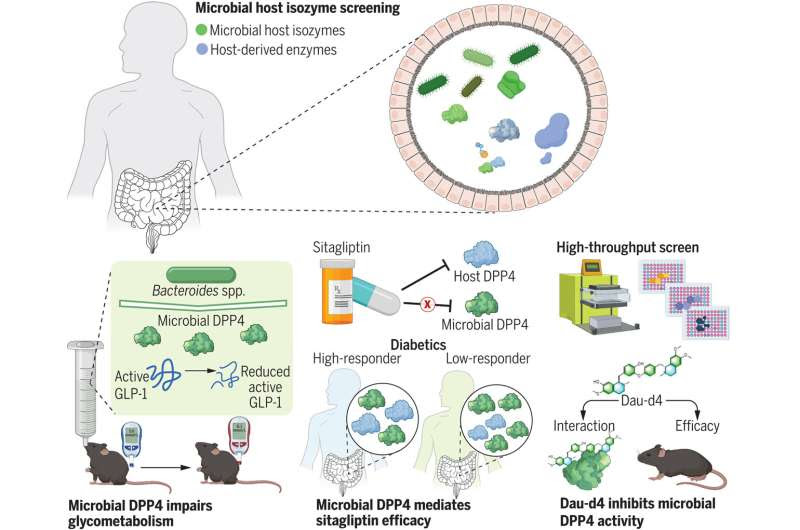
Discovery and inhibition of a gut microbial–host isozyme to regulate host metabolism. Differences in the gut microbiota may explain why some individuals respond to antidiabetic DPP4 inhibitors but others do not. An activity-based enzyme activity screening system identified gut microbial DPP4 isozymes that can decrease active GLP-1 but cannot be inhibited by sitagliptin. High-throughput screening identified Dau-d4 as a selective inhibitor of microbial DPP4 to increase GLP-1 activity and improve glucose tolerance. Credit: Science (2023). DOI: 10.1126/science.add5787
Research led by Peking University, China, has looked into gut microbiota production of isozymes, which do similar work to human enzymes but have different structures.
In a paper titled “Microbial-host-isozyme analyses reveal microbial DPP4 as a potential antidiabetic target,” published in Science, the team details interactions of microbiota isoenzyme cross-species regulation of metabolic disease surrounding type 2 diabetes, the diabetes drug sitagliptin and a compound derived from traditional Chinese medicine.
Gut microbiota can produce enzymes with functions similar to those produced by the body. These microbial isozymes can regulate physiology and pathophysiology as they assist or detract from regular enzyme interactions.
In searching for these interactions, the research team identified 71 enzymes with activity in human gut bacteria communities. They found species of Bacteroides producing microbial dipeptidyl peptidase 4 (mDPP4). The human version of DPP4 plays a significant role in regulatory processes such as T-cell homeostasis and metabolism. In the metabolism, DPP4 has a direct role in degrading the hormone GLP-1.
Glucagon-like peptide-1 (GLP-1) is a hormone that is released after eating a meal. GLP-1 decreases blood glucose by suppressing glucagon secretion and may be involved in glucose-dependent stimulation of insulin release. These actions lower blood sugar levels, which helps control type 2 diabetes and acts as an appetite suppressor. To increase the half-life and effectiveness of GLP-1 activity in type 2 diabetes patients, drugs like sitagliptin that inhibit DPP4 have been used.
In testing, researchers found that sitagliptin was not inhibiting the microbial-sourced mDPP4 isozymes. This unaffected source of mDPP4 enzyme activity, the researchers suggest, could be interfering with therapeutic drug treatments and drug trials in a microbiota-dependent manner.
In vitro, mDPP4 was found to be capable of degrading GLP-1. In a mouse model, the researchers gained further insight into the activity as mDPP4 did not affect functional GLP-1 levels in mice fed a regular chow diet. In mice fed a high-fat diet or subjected to treatment with conditions that result in a damaged gut barrier, mDPP4 decreased the activity of active GLP-1 and impaired glucose homeostasis. This implies that a damaged gut barrier is necessary for mDPP4 to impact the activity of host GLP-1 and influence blood glucose regulation.
The interaction between microbial DPP4 and Dau-d4 (a selective inhibitor)
High-throughput screening of over 100,000 compounds identified Dau-d4 as a selective inhibitor of mDPP4. Dau-d4, a derivative of daurisoline, selectively inhibited the activity of mDPP4 while sparing the inhibition of host DPP4.
Daurisoline is a compound derived from a traditional Chinese medicinal herb, Menispermum dauricum, a highly poisonous plant in its natural form. A series of daurisoline derivatives were obtained for preliminary study with Dau-d4, synthesized by methoxylation of the hydroxyl groups, showing improved inhibitory activity over the native molecule.
Dau-d4 was found to increase the levels of active GLP-1 and improve glucose metabolism in diabetic mice. When Dau-d4 was co-administered with the drug sitagliptin, it further enhanced blood glucose homeostasis, indicating a synergistic effect.
It should be noted that the modernization of traditional Chinese medicine is part of a proclaimed effort by the Chinese government. Traditional medicine is considered an essential achievement of Chinese civilization, and in 2016 the State Council issued the Outline of the Strategic Plan on the Development of Traditional Chinese Medicine.
As part of that stated national strategic goal, the State Council encourages the development of traditional Chinese medicine into new products with Western definable effects and the forming of modern industry applications with competitive advantages. Synergistic effects of traditional Chinese medicine with conventional Western treatments are considered crucial to bridging the gap between Eastern and Western methods and markets.
There are a few things to consider when cultural and governmental strategic goals attempt to intersect with science.
- Supporting research with enhanced funding levels could result in more scientific discovery, even the desired outcomes of more Western applications for traditional Chinese medicinal compounds.
- If governmental goals influence research parameters, the findings will also be limited by that influence. If researchers only test compounds derived from traditional Chinese medicine, then they will only find applications that work with compounds derived from traditional Chinese medicine, even if better options are available.
It also automatically raises the obvious implications of scientific bias that can arise when there is a drug or compound in search of something to cure. Thankfully for Chinese researchers, traditional Chinese medicinals have plenty of compounds to choose from.

Leave a Reply