By REBECCA DYER
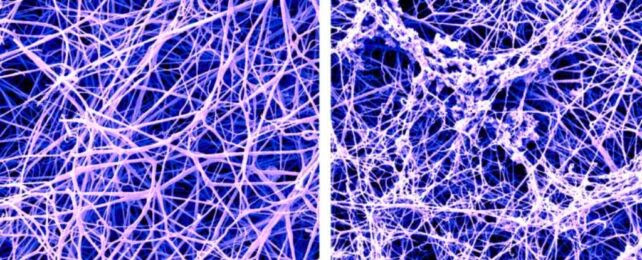
A false-color scanning electron microscope image of a fibrin blood clot before and after the buildup of protofibrils. (Anurag Sharma/Pradeep Singh)
Lecanemab received FDA approval in January after a phase 3 trial showed it slows cognitive decline in early-stage Alzheimer’s patients.
While we know lecanemab clears amyloid beta buildup, it was unclear how – but new research from the Rockefeller University in New York sheds some light on it. This could pave the way for new treatments for Alzheimer’s and other diseases.
“We believe we’ve found a mechanism that is one of the reasons lecanemab works,” says neurobiologist Erin Norris.
The drug seems to inhibit the plasma contact system; an interaction between proteins in the blood that helps promote clotting and inflammation. Though useful in repairing tissue damage, the system can cause harm when overstimulated in sensitive areas such as brain tissue, risking pathologies like Alzheimer’s disease.
“If you block the contact system, you’re going to get less Alzheimer’s pathology,” says neurobiologist Sidney Strickland.
Disorders of the brain – especially neurodegenerative diseases like Alzheimer’s – are among the most difficult medical puzzles to solve. Alzheimer’s disease affects millions of people worldwide, and there’s currently no cure.
Two important types of proteins, tau and amyloid beta (Aβ), clump into tangles and plaques in Alzheimer’s disease, leading to the death of brain cells and reduction in brain volume.
Aβ plaques can form from different types of clumps, of which protofibril are thought to be the most toxic. It’s these forms of the plaque that lecanemab targets.
Until recently, treatments aimed at clearing plaques from patients’ brains had not significantly slowed cognitive decline.
But patients who took lecanamab during an 18-month trial had a statistically significant drop in amyloid beta plaque in their brains compared to those who took a placebo, and it slowed cognitive decline by 27 percent.
As is unfortunately common, the treatment is not without adverse effects, including an increased risk of mild to moderate brain bleeds and swelling referred to as amyloid-related imaging abnormalities (ARIA). Compared to similar plaque-busting therapies, however, the risks are a relative improvement.
“It is noteworthy that lecanemab causes less ARIA (10 percent) than other anti-Aβ antibodies such as aducanumab (35 percent), gantenerumab (30 percent), or donanemab (27 percent),” the team writes in their paper.
The low ARIA rate of lecanemab piqued the interest of Norris, Strickland, and colleagues, who wanted to know why it was so effective.
Extensive analysis of plasma from eight donors without Alzheimer’s led them to discover that protofibrils are the only form of Aβ that are just the right size to activate the plasma contact system.
“It’s pretty amazing,” Norris says, “that the form of Aβ that specifically activates the contact system is the same form of Aβ that lecanemab targets.”
This activation of the contact system leads to overproduction of a peptide called bradykinin, which dilates blood vessels and can lead to the ARIA side effects that are more common with other anti-Aβ therapies.
Lecanemab appears to work by lowering Aβ accumulation and preventing protofibrils from activating the contact system, resulting in reduced bradykinin production.
The research team has developed an antibody called 3E8 that targets a circulating plasma protein for a similar outcome. They believe their findings mean 3E8 has potential for the treatment of Alzheimer’s disease, alone or in combination with medications like lecanemab, with possibly broader effects.
There’s a long way to go, but depending on its performance in clinical trials, the researchers think 3E8 could treat other diseases too.
“The dysregulation of the contact system is involved in COVID, sickle cell anemia, hereditary angioedema, inflammatory bowel disease, sepsis, lupus, arthritis, and even cancer metastasis,” Norris says.
The study has been published in the journal Proceedings Of The National Academy of Science.

Leave a Reply