Many questions remain about the formerly taboo chemicals that are being used to treat trauma and depression.
Sara Reardon
Psychedelic treatments are speeding towards approval — but no one knows how they work
Many questions remain about the formerly taboo chemicals that are being used to treat trauma and depression.
Conceptual illustration showing an abstract brain.

Illustration by Kasia Bojanowska
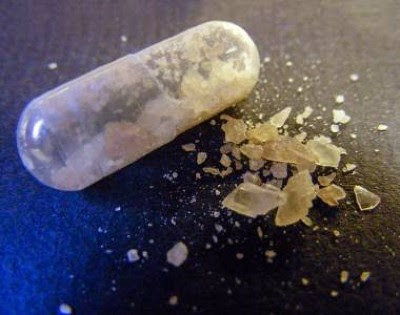
Psychedelic drugs have been undergoing a major makeover in psychiatry, earning mainstream acceptance that has eluded them for decades. In 2019, a variant of ketamine — an animal tranquillizer well known as a club drug — was approved by the US Food and Drug Administration (FDA) for treating post-traumatic stress disorder (PTSD). In May, Oregon opened its first treatment centre for administering psilocybin — the hallucinogenic compound found in magic mushrooms — following the state’s decision to legalize it (psilocybin remains illegal at the federal level). And, after decades of effort, the Multidisciplinary Association for Psychedelic Studies, a non-profit research organization in San Jose, California, formally asked the FDA for approval to market MDMA — also known as molly or ecstasy — as a treatment for PTSD.
Most specialists expect the MDMA approval to go through on the weight of clinical evidence and popular support. Two large trials have shown that the drug can reduce the symptoms of PTSD when administered in controlled therapy sessions1,2. And it seems to do so more quickly than other treatments. But how MDMA and other psychedelics work is still largely a mystery, both because the drugs have long been illegal and because psychiatric conditions are difficult to study in animals.

Psychedelic drug MDMA moves closer to US approval following success in PTSD trial
With the regulatory landscape shifting, legal psychedelic research is becoming easier — and potentially more profitable. Neuroscientists, psychiatrists, pharmacologists, biochemists and others are entering the field, bringing fresh ideas about what the drugs do at a cellular and molecular level and trying to unravel how these mechanisms might help to relieve symptoms of psychiatric conditions.
From a clinical perspective, understanding how the drugs work might not matter. “You don’t need to know the mechanism of the drug to have a very effective therapy,” says David Olson, a biochemist at the University of California, Davis. But, understanding more about psychedelics could lead to the development of proprietary drugs that are safer, less hallucinogenic and ultimately more effective. It could also affect the way psychedelics are administered in the clinic — helping providers to tailor treatments to each person.
Several key questions are driving the basic research that progresses in the background as MDMA and others march towards the market.
What is a psychedelic?
Indigenous cultures around the world have long used naturally occurring drugs such as psilocybin; peyote, which comes from a North American desert cactus; and ibogaine, extracted from the bark of a central-African shrub, to promote connectedness and open minds. Some evidence from the 1950s and 1960s suggested that these drugs and other synthetic compounds, such as ketamine or LSD, might have antidepressant effects3. But such research effectively ended in the late 1960s, when these substances were banned in most countries. The resurgence didn’t begin until the early 2000s, when clinical trials testing ketamine and, later, MDMA showed that the compounds worked at least as well as conventional psychiatric drugs1,4.
From a pharmacological viewpoint, the word ‘psychedelic’ historically refers to hallucinogenic drugs, including psilocybin and LSD, that bind to a serotonin receptor called 5-HT2A found on the surfaces of neurons. Although that definition does not include ketamine or ibogaine, these drugs have often been lumped together with psychedelics in research papers and public discourse. Even tetrahydrocannabinol, the active ingredient in cannabis, is sometimes considered a psychedelic.
This loose definition, combined with a lack of standardized reagents and protocols, can make it difficult for researchers to compare their work, says Bryan Roth, a pharmacologist at the University of North Carolina at Chapel Hill. “Much of what is being published is contradictory,” he says. But differences in the definitions of these drugs are only the beginning.
How do these drugs work?
Considered as a broad group, psychedelics, including ketamine and MDMA, are “fabulously dirty”, says Boris Heifets, an anaesthesiologist at Stanford University in California, meaning that they interact with many types of neuron and molecule across the brain. Even the classical psychedelics — such as LSD and psilocybin — interact with numerous receptors other than 5-HT2A. Studies differ on which are necessary for the drugs’ proposed psychiatric benefits.

Australia to prescribe MDMA and psilocybin for PTSD and depression in world first
“Honestly this is going to be something that’s going to be very difficult to unravel,” Olson says. The way that ketamine, for instance, might combat symptoms of depression and PTSD is mysterious. The drug binds to and blocks the NMDA receptor, a channel on the surface of neurons that is deeply tied to forming new connections. Blocking it triggers a parade of molecular events that had not previously been linked to depression.
Some studies suggest that a breakdown product of ketamine that binds to an as yet-unidentified receptor could cause antidepressant effects5. But an October study published in Nature6 found that ketamine can become trapped in the NMDA receptor and suppress activity in certain brain regions for up to 24 hours, which could account for the duration of its effects.
All psychedelic drugs might have something in common, even if they don’t use the serotonin receptor. In a paper published earlier this year7, neuroscientist Eero Castrén at the University of Helsinki and his team found evidence that psychedelics, including ketamine and psilocybin, all bind to the receptor for a brain signalling factor called brain-derived neurotrophic factor (BDNF), which is involved in neuron growth and brain rewiring. Conventional antidepressants, such as Prozac (fluoxetine), bind to the receptor, too, but the binding is up to 1,000 times stronger for psychedelics. That could explain why these drugs seem to improve symptoms in hours, whereas conventional antidepressants might take months, Castrén says.
Do psychedelics rewire the brain?
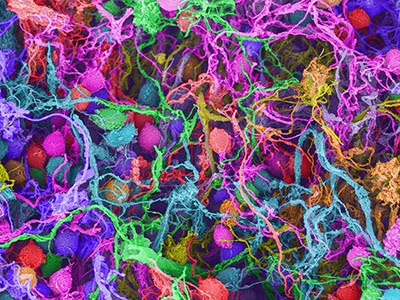
Although not everyone thinks that the BDNF receptor is the key, most scientists do think that psychedelic drugs promote brain plasticity, enabling the dendrites and axons that form neural circuits to diversify and make new connections. Plasticity could help a person with depression to see the world in a different way, or help a person with PTSD to disconnect their memories from a fear response.
But the nature of this plasticity and the brain regions involved are still hotly debated. “People talk about plasticity like there’s an understood meaning everyone agrees upon,” says Gerard Sanacora, a psychiatrist at Yale University in New Haven, Connecticut. “My concern is it’s replacing the ‘chemical imbalance’ catchphrase”, which was once broadly used to describe mental illness. “It’s a huge black box.”
A storefront for magic mushrooms, a type of mushroom that contains the drugs psilocybin or psilocin and causes hallucinations.
Although psilocybin mushrooms are illegal in Canada except for authorized clinical use, they are openly sold at retail outlets such as this one in Toronto.Credit: Creative Touch Imaging/NurPhoto via Getty

Plasticity isn’t necessarily a good thing either, says Lisa Monteggia, a neuroscientist at Vanderbilt University in Nashville, Tennessee. There are good reasons that the brain’s wiring develops in the way it does and maintains connections between experiences and effects. Some conditions, including autism and schizophrenia, might sometimes result from too much plasticity in the brain. Furthermore, all kinds of drug, including cocaine and amphetamines, can induce some sort of plasticity, Monteggia says.
Her group has been studying whether ketamine induces a particular type of plasticity one that allows neurons to regulate how active they are in the face of a stimulus that would normally affect them in a certain way. Unlike the plasticity mechanisms that strengthen or weaken specific neuronal connections during learning and memory, this homeostatic plasticity allows neurons to fight against factors that try to change them. In doing this, ketamine might give the brain the tools it needs to maintain a healthy state. If this mechanism turns out to be true, Monteggia says, ketamine might serve as a “Rosetta Stone” for understanding how other psychedelics work.
Gül Dölen, a neuroscientist at Johns Hopkins University in Baltimore, Maryland, meanwhile, doesn’t think psychedelics directly affect plasticity at all. Rather, she says, they might unlock something known as metaplasticity, making neurons more susceptible to a stimulus that induces plasticity — a hormone, for instance. This theory would put more importance on other factors — social interaction, for example, or reimagining a traumatic memory — in reshaping the neurons and forming new connections.
How psychedelic drugs achieve their potent health benefits
In a paper published in June in Nature8, Dölen’s group gave mice MDMA, ibogaine, LSD, ketamine or psilocybin while they were in the company of other mice. The treated mice became more willing to sleep in a compartment with others, and the effect lasted for weeks. Because adult mice don’t tend to change their social behaviour, Dölen says the finding suggests that psychedelics reopened a ‘critical period’ in which young mice learn to associate sociality with good feelings.
The team also found that the treated animals’ neurons started expressing a collection of genes involved in remodelling the protein network that exists outside cells, known as the extracellular matrix. This matrix acts as “grout” between neurons, Dölen says, and breaking it down frees dendrites and axons to form new connections.
What else might these drugs do?
Dölen says that psychedelics could be a “master key” that unlocks critical periods — making them more sensitive to particular stimuli. But much like plasticity, too much metaplasticity could be detrimental. Dölen says it would “melt the brain”: breaking hard-earned neural circuits, causing seizures and amnesia, and destroying the ability to learn. That’s why the stimulus connected to the drug experience — a social group for mice, for instance, or psychotherapy for humans — could be so important. That context might allow psychedelic therapies to circumvent the “melty brain problem”, Dölen says.
The implications could extend beyond psychiatric conditions. Dölen’s laboratory is currently testing whether psychedelics can open other critical periods in mice. Opening a critical period in the motor cortex, for instance, might lengthen the amount of time in which people who have had strokes can benefit from physical therapy. Psychedelics might help people to recover lost or impaired senses or even learn a new language, given the right conditions.
Taking the tripping out of psychedelic medicine
If context is essential, the hallucinogenic experience itself might be necessary to open critical periods. “The altered state invites all the different ways of thinking about things,” says Rachel Yehuda, a psychiatrist at the Icahn School of Medicine at Mount Sinai in New York City. Her group is studying the use of MDMA and psilocybin in people with PTSD, which the researchers think helps people to open up about traumatic experiences and address them in ways they normally couldn’t.
Yehuda’s work has found that psychedelic treatment adds chemical markers to genes involved in psychiatric conditions9, although she is quick to add that psychotherapy can cause the same kind of ‘epigenetic changes’. “You do not have to ingest a drug to have a neurochemical change, we have neurochemical changes all the time,” she says. The drug might simply enhance the therapy’s ability to change a person’s perspective permanently. “Clinically, we know there is more to the story than the way a compound is hitting a certain receptor,” Yehuda says. “We don’t have a full story and I don’t think anyone does.”
But others think that the direct effects of psychedelics on the brain are responsible for their efficacy. Olson’s lab has found that chemical compounds derived from ibogaine and other drugs can increase neuroplasticity and decrease drug-seeking behaviour and depression in mice without causing hallucinations10. Inducing this kind of neuronal growth, he says, might be sufficient for some people, whereas others would benefit from psychotherapy or a transcendent experience. “These are questions that can only be answered in the clinic,” he says.
Is it all a placebo effect?
Clinically testing a psychiatric drug against a placebo has always been hard — recipients want it to work, which can affect their level of depression. That’s even worse when the drug creates an intense effect, making it unlikely that a study participant would mistake a placebo for the real thing. The FDA has approved a system for MDMA trials in which psychiatrists, who are not involved with administering therapy, evaluate the improvement in each person’s symptoms without knowing who received the drug. The agency is therefore waiving its usual requirement to conceal treatment status from participants and the physicians administering the drugs during trials.
Heifets might have found a way to test the intensity of the placebo effect. In a small study11 posted on the preprint server medRxiv in June, his team tested ketamine in people undergoing surgery who were put under anaesthesia and unable to experience the drug’s dissociative effects. People coming out of surgery often experience heightened symptoms of depression. But the researchers found that regardless of whether a patient received ketamine or a placebo, their symptoms improved if they thought they might be getting the drug.

How ecstasy and psilocybin are shaking up psychiatry
Although Heifets isn’t entirely sure why the placebo worked as well as ketamine, he suspects that the expectation of receiving the drug itself might have improved their mood. That’s not necessarily a bad thing or “just a placebo effect”, he says. After all, if a person’s symptoms improve, it suggests that something is changing in their brain. “What our data strongly suggest is that non-drug factors are powerful mediators,” Heifets says. “It forces a bit of reconsideration of what ‘placebo’ means.”
Sanacora agrees: the expectation of receiving a drug could be one of many factors — both psychological and biochemical — that contribute towards psychedelics’ overall effectiveness. “We’d be very naive to not realize that expectations play a large role,” he says.
The real test will come with drugs that are similar to psychedelics but don’t induce strong effects, including hallucinations. Olson’s team and his start-up company, Delix Therapeutics in Boston, Massachusetts, are among those developing spin-off drugs that target the same brain pathways as psychedelics and cause plasticity without the trip. Several of these drugs, derivatives of ibogaine, LSD or other psychedelics, are now in clinical trials to determine whether they can treat mental illnesses. If they have the same clinical benefits, Olson says, they could be useful for certain people, including those with psychiatric conditions that can be triggered by an emotional experience. They could also avoid some side effects, such as heart conditions linked to drugs such as MDMA.
From a more practical standpoint, pharmaceutical companies can’t patent a drug such as LSD, but they could patent a derivative with the same mechanism of action. A new drug with a known mechanism would be easier to regulate as well — agencies such as the FDA still worry about the potential for abuse with party drugs such as ketamine and MDMA.
Wherever the psychedelic business ends up, these mind-expanding drugs might broaden researchers’ thinking about concepts such as neuroplasticity, psychology and the wiring of the brain. “What excites me most about psychedelics is they’re incredibly useful tools for understanding the basic biology of the brain,” Olson says.
Nature 623, 22-24 (2023)
doi: https://doi.org/10.1038/d41586-023-03334-6

Leave a Reply