by University of Hawaii at Manoa
Credit: Molecular Therapy – Nucleic Acids (2023). DOI: 10.1016/j.omtn.2023.07.032
Gene therapy has great promise for treating genetic diseases, and even for more common diseases such as atherosclerosis (hardening of the arteries). Over the past decade, the gene-editing technology CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats)—a family of DNA sequences found in the genomes of certain bacteria—has allowed scientists to fix individual errors in the genetic code that cause disease.
However, the delivery of gene therapy using viral methods (using non-disease-causing viruses to deliver a healthy copy of a gene) poses safety concerns while current non-viral methods are limited by low efficiency.
In the Center for Cardiovascular Research at the University of Hawaiʻi at Mānoa John A. Burns School of Medicine (JABSOM), former graduate student and postdoctoral researcher, Cynthia Anderson, has made progress using a less invasive process. In a recent study published in Molecular Therapy—Nucleic Acids, she used ultrasound and microbubbles to deliver CRISPR tools to the liver to inactivate a gene that increases cardiovascular risk.
Gene inactivation process
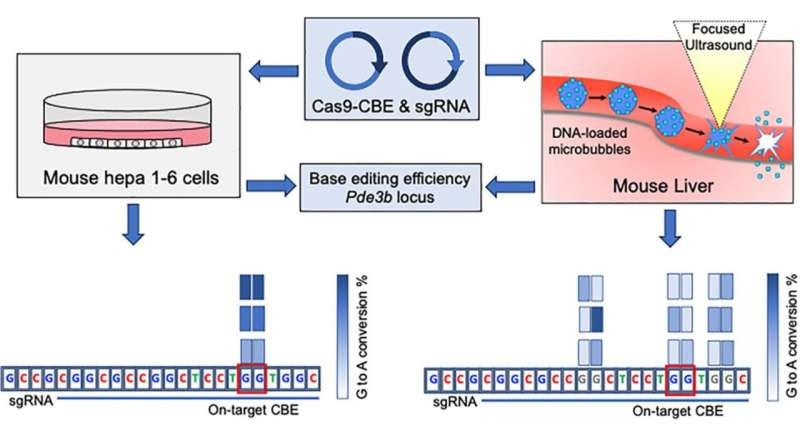
Working with her mentor, Ralph Shohet, director and professor at the Center for Cardiovascular Research, and collaborators at Stanford University, Anderson mixed plasmids (small circular DNA molecules ) that encode the proteins and DNA needed to change a gene sequence, with microbubbles that are commonly used for contrast in echocardiography.
She then injected this mixture of bubbles and DNA into mice and exposed the liver to high intensity focused ultrasound as the bubbles moved through the liver. When the bubbles popped, the plasmids were transferred to the liver cells.
“There they changed the genetic code of the PDE3B gene, which encodes a protein important in inflammation and lipid metabolism, in a way that inactivated the protein. This inactivation is known to lower triglyceride levels and to protect against cardiovascular disease in humans,” explained Shohet.
In this proof-of-principle experiment, Anderson also showed that changing DNA sequence in the living animal was less accurate than in cell culture, using the exact same CRISPR plasmids.
“This is important as we often evaluate the effects of gene therapy first in cell culture, and Anderson’s experiment emphasizes that we need to be particularly careful of how the same therapies will work in animals, and eventually in humans,” said Shohet.
More information: Cynthia D. Anderson et al, Non-viral in vivo cytidine base editing in hepatocytes using focused ultrasound targeted microbubbles, Molecular Therapy—Nucleic Acids (2023). DOI: 10.1016/j.omtn.2023.07.032
Provided by University of Hawaii at Manoa

Leave a Reply