by McMaster University
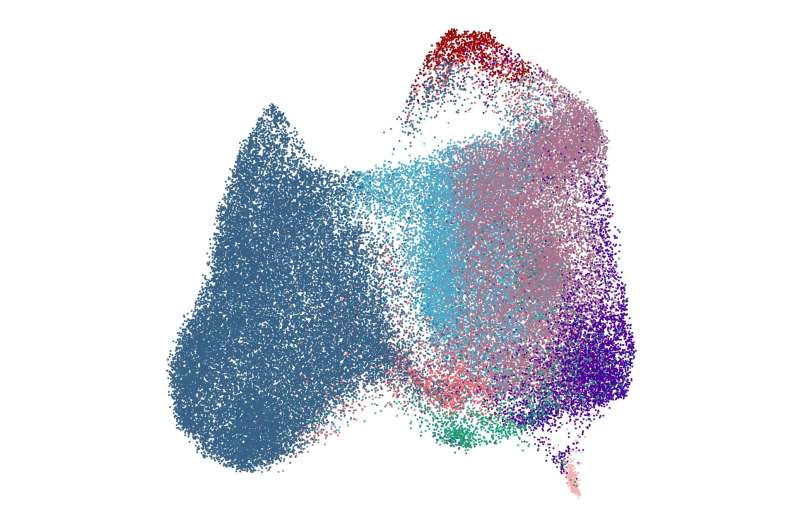
Image depicting UMAP of mass cytometry data analyzing human B cell subsets. Credit: Depiction generated by David R. Glass, project lead by Joshua F.E. Koenig, Peter Sejer Andersen, Niels Peter H. Knudsen, Allyssa Phelps, and Kelly Bruton.
Researchers with McMaster University and Denmark-based pharmaceutical company ALK-Abello A/S have made a groundbreaking discovery: a new cell that remembers allergies.
The discovery gives scientists and researchers a new target in treating allergies and could lead to new therapeutics. The research, published in Science Translational Medicine, coins the brand-new cell as a type-2 memory B cell (MBC2).
“We’ve discovered a type of memory B cell that had unique characteristics and a unique gene signature that has not been described before,” says Josh Koenig, assistant professor with McMaster’s Department of Medicine and co-lead of the study. “We found allergic people had this memory B cell against their allergen, but non-allergic people had very few, if any.”
B cells are a type of immune cell that makes antibodies. These cells help fight off infections but can also cause allergies.
“Let’s say you’re allergic to peanuts. Your immune system, because of MBC2, remembers that you’re allergic to peanuts, and when you encounter them again, it creates more of the antibodies that make you allergic,” Koenig says.
To come to this discovery, researchers created tetramers—a type of fluorescent molecule—out of allergens like Birch pollen and peanuts to locate difficult-to-find memory B cells. Koenig and his team previously wrote the instruction manual on how to use tetramers to locate these elusive cells.
Researchers further leveraged samples from ALK clinical trials with tablet sublingual immunotherapy, which allows for sequencing large amounts of IgE-producing B cells.
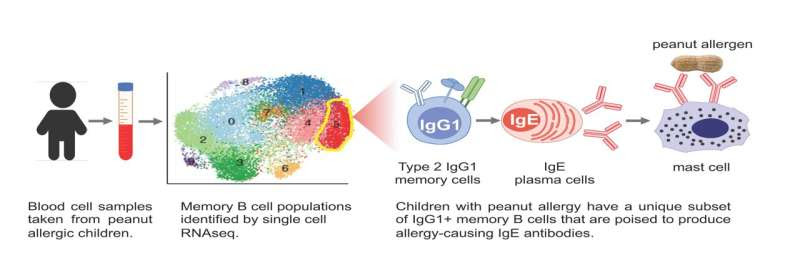
Using cutting-edge technology such as single-cell transcriptomics and deep sequencing of antibody gene repertoires on clinical trial samples, they were able to make direct connections between MBC2 and IgE, the type of antibody that triggers the allergic reaction. This provided necessary context, ultimately revealing the MBC2 as the home of allergy.
Researchers discover new cell that remembers allergiesSchematic illustrating how the researchers examined blood samples from children with peanut allergies to identify the origin of allergy-causing IgE antibodies. The findings uncovered a a population of type 2-imprinted IgG1 memory B cells that express CD23, IL4R and germline IGHE, and are primed to switch to IgE. Credit: Mariana Waldetario, Marie Anne O’Donnell and Maria Lafaille.
“Even though allergies are the most prevalent disease worldwide, it is still not fully understood how allergy occurs and evolves into a life-long condition. Finding the cells that hold IgE memory is a key step forward and a game-changer in our understanding of what causes allergy and how treatment, such as allergy immunotherapy, can modify the disease,” says Peter Sejer Andersen, senior vice-president and head of research at ALK. Sejer Andersen co-led the study with Koenig.
“We are very excited about this finding and grateful to the team at McMaster University for an excellent and productive collaboration.”
The discovery of MBC2 gives scientists and researchers a new target in treating allergies and could lead to new therapeutics.
“The discovery really pinpoints two potential therapeutic approaches we might be able to take,” says Kelly Bruton, who co-led the research alongside Koenig when she was a Ph.D. student at McMaster. Bruton is now a postdoctoral fellow at Stanford University.
“The first is targeting those MBC2s and eliminating them from an allergic person. The other option could involve changing their function and have them do something that’s not going to be ultimately harmful when the individual is exposed to the allergen.”
Further work will be needed to better understand and ultimately create therapeutics, but the discovery of MBC2s offers new hope for those affected by food allergies.
“These are the types of discoveries that you really need to make in order to develop the right therapeutics to block the right cells to stop the disease,” Koenig says.
The research was also co-led by Niels Peter Knudsen and Allyssa Phelps. Manel Jordana, a professor of medicine at McMaster, is also cited by Koenig as being integral to the discovery.
More information: Joshua Koenig et al, Type 2 Polarized Memory B cells Hold Allergen-Specific IgE Memory, Science Translational Medicine (2024). DOI: 10.1126/scitranslmed.adi0944. www.science.org/doi/10.1126/scitranslmed.adi0944
Journal information: Science Translational Medicine
Provided by McMaster University

Leave a Reply