By Theresa Gaffney
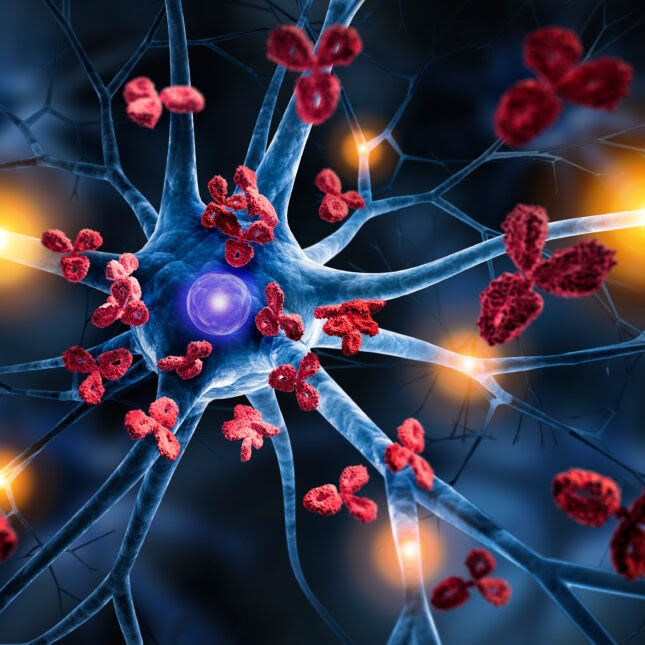
ADOBE
People with autoimmune disorders don’t usually get to talk about a cure. There’s symptom management, hopeful periods of remission often followed by relapses, but rarely a lasting fix for the way their immune system attacks healthy cells. If the immune system is an army, then those with conditions like lupus, multiple sclerosis, or rheumatoid arthritis are often fighting a never-ending war of friendly fire.
But over the last few years, researchers in Germany have begun testing the potential of CAR-T therapy — a cutting-edge cancer treatment in which a patient’s immune T cells are genetically modified in a lab to better attack disease targets — to help those with autoimmune disorders. Their latest findings, published Wednesday in the New England Journal of Medicine, provide evidence that has led experts to consider, tentatively, using the c-word.
In a study of 15 patients — eight with lupus, four with systemic sclerosis (scleroderma), and three with idiopathic inflammatory myositis, a rare muscle disease — researchers eliminated or reduced symptoms and disease biomarkers with a single infusion of CAR-T cells designed to target B cells, immune cells that play a key role in driving autoimmunity. There were no relapses among lupus patients, who were monitored for up to two years after treatment. The myositis and sclerosis patients, who had shorter-term follow-up (usually about three to six months but up to a year) saw their symptoms significantly lessen.
“It’s wonderful. I mean, some people would think that this might be too good to be true, but it actually does look true,” said Carola Vinuesa, an immunologist and geneticist at the Francis Crick Institute in London, who was not involved with the research.
Related: CAR-T, recently used in a lupus patient, helps other autoimmune patients, too, in small study
Patients included in the case study were experiencing severe forms of these diseases that affected at least two organs, with “not many treatment options left,” according to Fabian Müller, a hematologist-oncologist at University Hospital Erlangen and first author on the paper.
For patients with myositis, muscles are damaged by elevated levels of an enzyme called creatine kinase. Extreme disease can leave a person bedridden, struggling to breathe. One of the team’s patients with myositis, a 42-year old man, could barely stand before treatment and was only able to walk about 30 feet. Two or three months later, he was walking so much that he reported foot pain at a follow-up appointment, because his bones hadn’t yet gotten used to his stronger muscles, Müller said. Now, that patient walks 6 miles to work each day, just because he can, he said.
A patient with lupus, which can affect joints, skin, kidneys, lungs, and more, was experiencing heart failure before treatment. But afterward, her fatigue and other symptoms disappeared and she’s back to life as normal. A patient with scleroderma, which makes someone’s skin tight, hard, or stiff, is walking confidently again now that he feels like he is standing on steady ground once more.
The findings build on results the researchers presented at the annual American Society of Hematology meeting late last year. When the team first began publishing their research, experts were cautiously intrigued. Before the infusion of CAR-T cells, patients receive chemotherapy to prepare and clear their immune system. It was possible that early positive results were simply due to the proven benefits of chemo. But now, with positive results lasting for as long as two years, it’s becoming more clear that the therapy is driving the improvements.
But it’s still unclear exactly why the CAR-T therapy seems to work so much better than previous treatments that target B cells using monoclonal antibodies. Perhaps an antibody “doesn’t have the ability to actively traffic into tight spaces and can only see what’s in the blood or what’s getting a lot of blood, whereas the CAR-T cells have access to other tissues,” said Mark Leick, a physician at the Hematopoietic Cell Transplant and Cell Therapy Program at Massachusetts General Hospital.
Previous monoclonal antibody therapies target B cells via a protein they carry known as CD20. Müller and his team made CAR-T cells that would target B cells carrying a different protein, CD19. This difference could be part of the “deeper depletion” of B cells seen in CAR-T therapy, said John Isaacs, a rheumatologist and professor at Newcastle University who wrote a commentary on the study also published Wednesday in NEJM. Alternatively, CAR-T cells could simply be more lethal than antibodies, he said.
Critically, patients did not appear to lose immunity to diseases they’d previously been vaccinated against, “which is like a dream,” said Vinuesa. The team did observe a decrease in the level of SARS-CoV-2 antibodies in patients’ bodies after treatment, but two patients who received vaccines afterward saw those levels rise.
Experts say it’s still too early to label CAR-T therapy as a real cure for the autoimmune disorders. Still, “it does look like probably the best treatment there’s been,” Vinuesa said. Patients who took handfuls of pills every day before are now treatment-free. “It definitely gives [the patients] an incredible break from disease.”
Longer term follow-up on bigger groups of patients is needed, which researchers across the globe are now racing to perform, said PJ Utz, a physician who runs a research lab at Stanford University studying autoimmunity. He knows of three companies pursuing CAR-T therapy for autoimmune disorders, including Kyverna Therapeutics, which filed for its initial public offering last month.
“I’ve been working on these diseases for 30 years now. And we always say, ‘We want to cure them, we want to cure them.’ We’ve never had anything like this where a disease completely disappears,” said Utz, who was not involved in the study.
As for the team of researchers pioneering the research, they aren’t legally able to form any company, Müller said, because they are using technology from German biotech Miltenyi to build the chimeric antigen receptors (CAR) and produce them in patient T cells. Still, they’re working on a Phase 1/2 expansion trial with another two dozen patients and longer follow-up periods, Müller said.
“There will be relapses coming. We’re sure it can’t be that good,” he said of the treatment. Part of the team’s continuing research will be figuring out how to address those relapses.
In cancer treatment, patients are considered cured if their disease hasn’t returned after five years off all therapy. And since CAR-T is a treatment borrowed from cancer, perhaps rheumatologists should consider adopting that same definition for a cure, Utz said. Müller noted that he would consider lupus patients cured three to five years after stem cell transplants. By either definition, most of the patients in this study may be on their way.

Leave a Reply