JULY 11, 2024
by University of Warwick
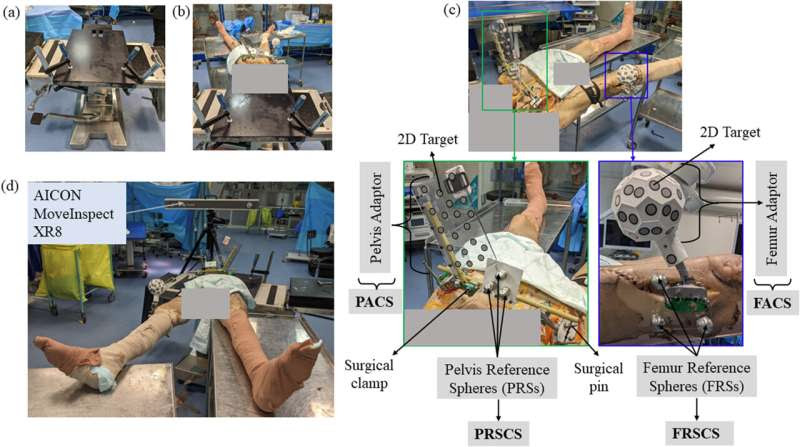
Experimental set-up for the cadaver experiment. (a) A specially designed fixation plate is used to position the cadaver specimen. (b) The cadaver specimen is secured to the fixation plate using a C-clamp, and the fixation plate is clamped onto a height-adjustable table. (c) ‘Pelvis Adaptor’ and pelvis reference spheres (PRSs) are attached to the pelvis. They serve to establish the pelvis adaptor coordinate system (PACS) and pelvis reference sphere coordinate system (PRSCS), respectively. Similarly, ‘Femur Adaptor’ and femur reference spheres (FRSs) are affixed to the femur, providing the femur adaptor coordinate system (FACS) and femur reference sphere coordinate system (FRSCS), respectively. Surgical clamps, pins, and plastic glue are employed to secure these attachments to the pelvis and femur. (d) The final experiment setup is depicted, along with the positioning of the AICON MoveInspect XR8 during the experiment. Credit: Computers in Biology and Medicine (2023). DOI: 10.1016/j.compbiomed.2023.107799
“Personalized” hip replacement surgery might be just what the doctor ordered for people with hip arthritis—according to new research. Using advanced technology from other industries such as automotive and manufacturing, researchers are driving medical advancement.
The result is tailored hip replacements, as each person moves their hips in slightly different ways. At the moment, replacements are based on a “normal” hip rather than being specifically designed for the patient.
In the study by WMG at The University of Warwick, in collaboration with University Hospitals Coventry and Warwickshire (UHCW) NHS Trust and Corin Group, researchers revealed that this pioneering approach to hip replacements could improve patient outcomes and surgery success rates.
The paper is published in the journal Computers in Biology and Medicine.
More than 100,000 people in the UK undergo hip replacements each year, according to the NHS—commonly due to arthritis, a disease of the joints that causes significant pain.
The new study analyzed longstanding problems in hip replacement surgery: on the specific range of motion needed in a replacement and how the value of the personalized surgery could be calculated before any operation.
In the study, Lead Researcher Dr. Arnab Palit, Assistant Professor at WMG at The University of Warwick, and his team combined real-life and computer models to compare simulated and real hip motions.
This demonstrated that certain hip motions can be easily and accurately calculated using state-of-the-art computer simulations based on CT scans of the patient’s hip joint, closely mirroring real hip motions.
This advancement could enable surgeons to plan hip surgeries based on patient-specific target hip motions, rather than relying on population norms or arbitrary “normal” values. This personalized approach is particularly valuable for patients who do not fall within these average values, ensuring that pre-surgical planning is truly individualized and likely to be more effective.
Using these tailor-made hip replacements could improve the success of operations, making them “right at the first time.” Surgeons may be able to put the artificial hip in just the right spot based on the pre-operatively calculated personified target hip motion.
This could reduce the chances of any clinical problems later on, minimizing the risk of revision surgery. This will also help to improve the recovery time of patients, while also reducing additional costs and labor to the NHS.
Dr. Palit said, “This research shows a big step forward in hip replacement planning. By using computer simulations based on a patient’s hip shape from CT scans, we can predict certain hip movements accurately. During surgery, these predicted movements can guide them to place implants in the best positions for each patient.
“So, instead of using average measurements, we’re customizing the surgery to fit each person perfectly, leading better surgery. Further research will be necessary to fully explore its potential to utilize it for NHS patients.”
Professor Richard King, Clinical Orthopaedic Surgeon at UHCW and the clinical lead of the project, commented, “The hip replacement has been called “the operation of the century. As surgeons, we are constantly looking to make it better and more reliable. This work we have done with WMG could help us to do exactly this, by showing us how to tailor the operation precisely for each individual patient.”
Dr. Christopher Plaskos, Vice President, Global Clinical Innovation at Corin Group, added, “Corin is proud to support this research aimed at predicting the true range of clinical motion of a hip joint from pre-operative CT and hip motion simulation. It’s research like this that will shape the future of hip planning, leading to truly personalized hip replacement.”
More information: Arnab Palit et al, Evaluating computed bony range of motion (BROM) by registering in-vitro cadaver-based functional range of motion (FROM) to a hip motion simulation, Computers in Biology and Medicine (2023). DOI: 10.1016/j.compbiomed.2023.107799

Leave a Reply