by Tohoku University
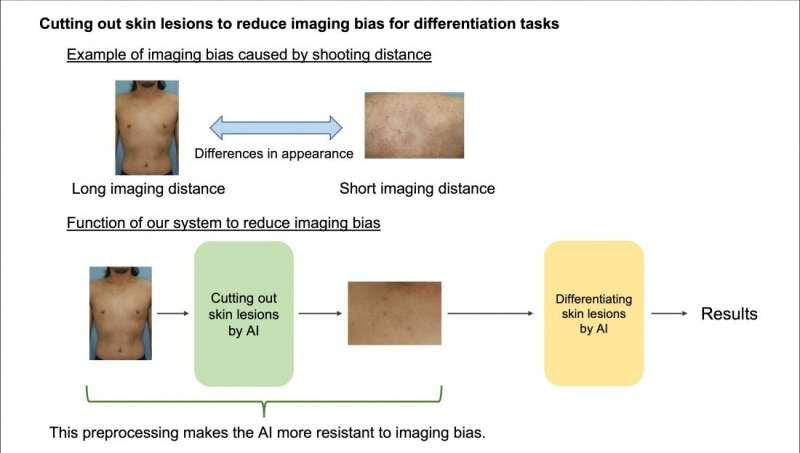
Images of skin lesions can vary significantly depending on the distance between the lesion and the imaging device. By minimizing the imaging bias caused by distance, the accuracy of skin lesion differentiation can be enhanced. Credit: Yuta Yanagisawa et al
Atopic dermatitis skin lesions and the lesions produced by infectious complications of the disease look so similar that it makes it impossible for patients to spot the difference and know when to visit their doctor for treatment. But an AI-powered mobile app developed by dermatologists now puts the power of diagnosis in the hands of patients.
A team of dermatologists has developed an artificial intelligence (AI) model that empowers atopic dermatitis (AD) patients to detect complications from bacterial or viral infections and distinguish between eczema and skin lesions caused by a type of blood cancer.
The AI model is detailed in a paper published in the Journal of Dermatological Science on January 10, 2023.
AD is a chronic disease that affects about 12% of people and often begins in childhood. Patients with AD typically have a suppressed skin immune barrier, which reduces their protection against microbial pathogens, leading to complications of the eczema from bacterial or viral infections. This may include herpes simplex, impetigo, and Kaposi varicelliform eruption (eczema herpeticum).
Recognizing whether AD has led to any of these complications can be challenging for patients as the symptoms’ appearance on the skin is very similar to AD itself. Moreover, mycosis fungoides, a type of blood cancer that causes skin lesions, can also exhibit similar symptoms to AD and may co-exist with AD. Some medications for AD can even worsen infections or mycosis fungoides.
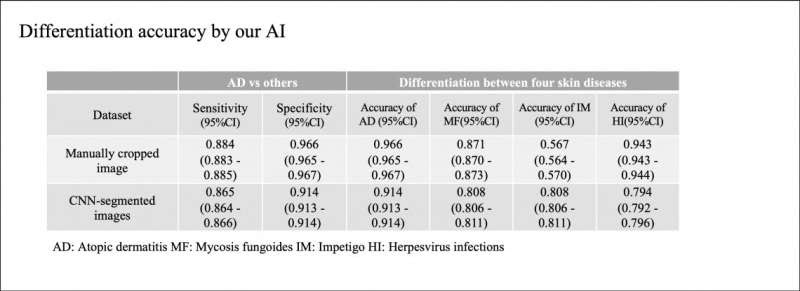
Our system achieved an accuracy rate almost equivalent to that of dermatologists when cropping skin lesions for differentiation. Credit: Yuta Yanagisawa et al
Proper and early diagnosis of complications and malignant diseases is critical for appropriate treatment and better outcomes. However, patients cannot always recognize any abnormal symptoms and visit a doctor as soon as possible due to the similarity of symptoms.
To address this issue, the team trained their convolutional neural network (CNN) model on non-standard images of AD, impetigo, mycosis fungoides, herpes simplex, and Kaposi varicelliform eruption. They then compared the AI’s diagnosis accuracy to a set of non-standard images manually cropped and diagnostically annotated by dermatologists. They found that their system achieved a diagnostic accuracy almost equal to the manually assessed image set.
The team is currently developing an AI powered smartphone app to translate their system, enabling patients to manage their skin diseases remotely with just their phone’s camera. They are also experimenting with AD patients to improve the app’s usability.
Yuta Yanagisawa, a researcher with the Tohoku University School of Medicine and co-author of the paper, said, “A dermatologist would of course be able to spot the difference, but it is incredibly impractical for an AD patient to visit a dermatologist every day. If only there were some handy, low-cost mechanism that replicated that dermatologist’s knowledge and could be used during a patient’s daily regimen of checking their skin.”
The team believes that this technology will help patients with skin diseases to manage their conditions effectively and efficiently, resulting in better health outcomes.

Leave a Reply