By Paul McClure
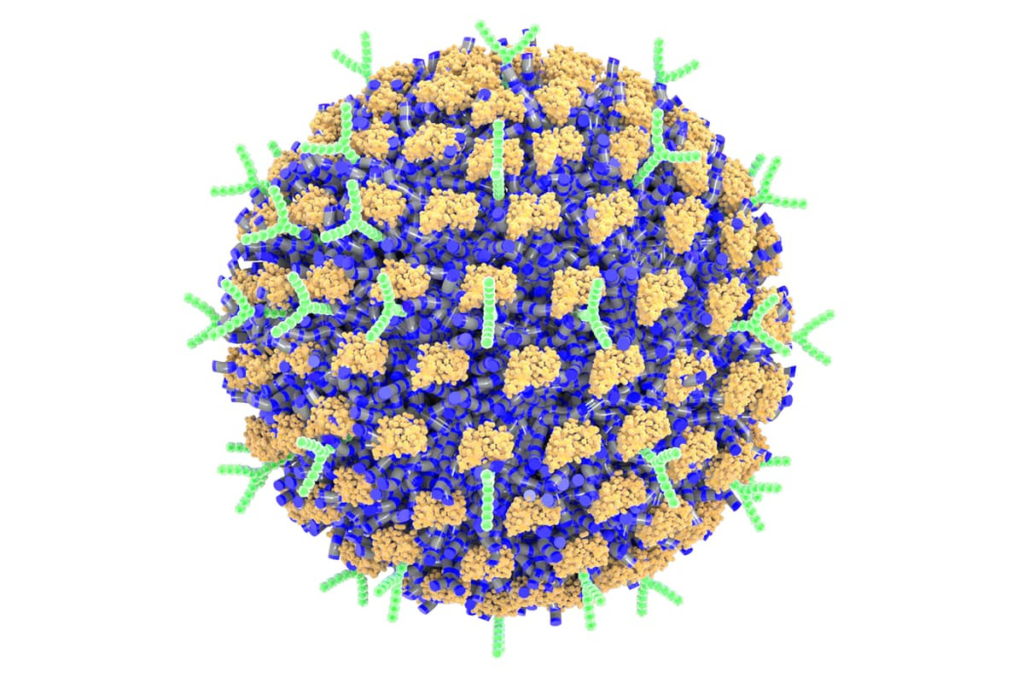
Researchers have created a nanoparticle decorated with antibodies that targets the cells responsible for allergic reactionsEvan A. Scott/Northwestern University
Researchers have created a nanotherapy that selectively targets and shuts down the immune cells responsible for causing an allergic response in mice, preventing anaphylaxis. Able to be tailored to specific allergens, the novel nanomedicine could be the first to prevent allergic reactions.
Allergies can range in severity from itchy eyes and a runny nose to life-threatening anaphylaxis. Peanuts, dust, mold, dog hair, perfume, pollen, drugs, insect stings, and latex – besides avoiding these things entirely, for some people there’s no way to prevent allergic reactions.
That may soon change, thanks to researchers at Northwestern University who’ve developed the first selective therapy to prevent allergic reactions: nanoparticles decorated with antibodies that shut down the immune cells responsible for the body’s allergic responses.
“Currently, there are no methods available to specifically target mast cells,” said Evan Scott, corresponding author of the study. “All we have are medications like antihistamines to treat symptoms, and those don’t prevent allergies. They counteract effects of histamines after the mast cells already have been activated. If we had a way to inactivate the mast cells that respond to specific allergens, then we could stop dangerous immune responses in severe situations like anaphylaxis as well as less serious responses like seasonal allergies.”
Mast cells are tissue-resident white blood cells that are essential to allergic inflammation. When someone becomes allergic, their mast cells capture and display antibodies, specifically immunoglobulin E (IgE), for that specific allergy-triggering substance – an allergen, almost always a protein. This enables mast cells to recognize and react to the same allergen if the person is re-exposed to it.
“If you have a peanut allergy and have had a response to peanuts in the past, then your immune cells made IgE antibodies against peanut proteins, and the mast cells collected them,” said Scott. “Now, they are waiting for you to eat another peanut. When you do, they can respond within minutes, and if the response is strong enough, it can result in anaphylaxis.”
For proteins, such as antibodies, to stick to a nanoparticle, they typically must form a bond that unfolds the protein, affecting its bioactivity. To address this challenge, the researchers created a nanoparticle comprised of dynamic polymer chains that can independently change their orientation when exposed to different solvents and proteins. So, when a protein is attached to the surface of the nanoparticle, the polymer chains at the interface flip their position to hold onto the protein stably without bonding to it, thereby retaining its function. Water-repelling pockets on the protein’s surface were key to maintaining a stable interaction.
“This is a uniquely dynamic surface,” Scott said. “Instead of a standard stable surface, it can switch its surface chemistry. It’s made of tiny polymer chains of compounds, which can flip their orientation to maximize favorable interactions with both water and proteins as necessary.”
The researchers found that close to 100% of antibodies attached to the nanoparticles without losing their ability to bind to their specific targets, resulting in a nanoparticle whose surface was densely packed with highly controllable amounts of multiple distinct mast-cell-targeting antibodies.
Scanning electron microscopy (SEM) image of the nanoparticles (colorized in purple) inside a mast cell
Scanning electron microscopy (SEM) image of the nanoparticles (colorized in purple) inside a mast cellEvan A. Scott/Northwestern University
The nanoparticle is decorated with anti-Siglec-6 antibodies that prevent mast cells from reacting to an allergen. It also carries allergens that correspond to a person’s particular allergy. For example, if the nanoparticles were being used on a person with a peanut allergy, they would carry a peanut protein. It’s a two-pronged approach: the allergen engages the specific mast cells responsible for the allergy, and then the antibodies shut down those cells. And because only mast cells display Siglec-6 receptors, the nanoparticle can’t bind to other cell types, effectively limiting side effects.
“You can use any allergen you want, and you will selectively shut down the response to that allergen,” Scott said. “The allergen would normally activate the mast cell. But at the same time the allergen binds, the antibody on the nanoparticle also engages the inhibitor Siglec-6 receptor. Given these two contradictory signals, the mast cell decides that it shouldn’t activate and should leave that allergen alone. It selectively stops a response to a specific allergen. The beauty of this approach is that it does not require killing or eliminating all the mast cells. And, from a safety standpoint, if the nanoparticle accidentally attaches to the wrong cell type, that cell just won’t respond.”
After successfully using the novel nanoparticle on human-tissue-derived mast cell cultures, the researchers tested the therapy on mouse models. Because mast cells in mice don’t possess Siglec-6 receptors, the researchers developed a model with human mast cells in their tissues. The mice were exposed to an allergen, and the nanotherapy was simultaneously delivered intravenously. None of the animals experienced anaphylaxis, and all survived.
“The simplest way to monitor an allergic reaction is to track changes in body temperature,” said Scott. “We saw no changes in temperature. There was no response. Also, the mice remained healthy and did not display any outward sign of an allergic reaction.”
The researchers next plan to use their nanotherapy to treat other mast-cell-related diseases, including a rare form of mast cell cancer called mastocytosis. They’re also investigating loading drugs inside the nanoparticles to selectively kill mast cells in mastocytosis without injuring other cell types.
They see that their nanotherapy has a number of applications.
“The biggest unmet need is in anaphylaxis, which can be life-threatening,” said Bruce Bochner, a study co-author. “Certain forms of oral immunotherapy might be helpful in some cases, but we currently don’t have any FDA-approved treatment options that consistently prevent such reactions other than avoiding the offending food or agent. Otherwise, treatments like epinephrine are given to treat severe reactions – not prevent them. Wouldn’t it be great if there was a safe and effective treatment for food allergy that consistently made it possible to reintroduce a food into the diet that you used to have to strictly avoid?”
The study was published in the journal Nature Nanotechnology.
Source: Northwestern University

Leave a Reply