by Society for Healthcare Epidemiology of America
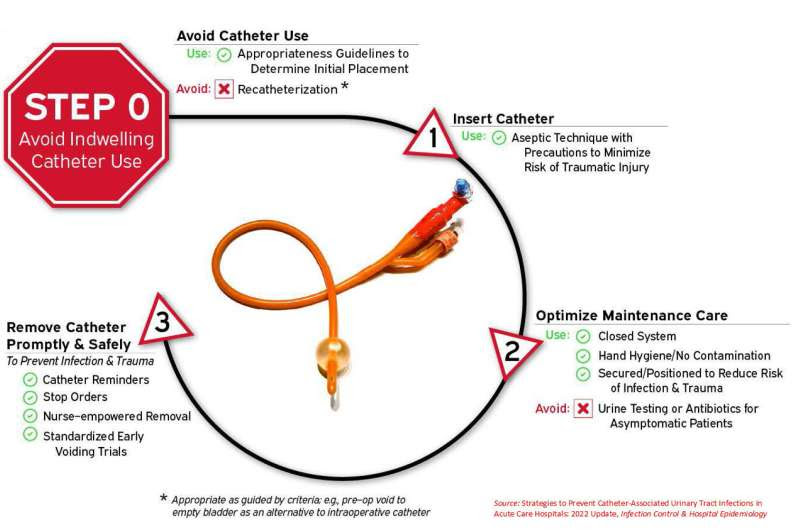
Alternatives to indwelling urinary catheters help patients avoid infections and urethral traumaAvoiding the unnecessary use of indwelling catheters and promptly removing catheters that are no longer needed are the first steps in preventing catheter-associated urinary tract infections in acute care hospitals, according to new recommendations. The model, “Disrupting the Lifecycle of the Urinary Catheter,” identifies alternatives to indwelling catheters, shows how to follow guidance for safely inserting and maintaining catheters, and prompts healthcare personnel to initiate timely removal. Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals: 2022 Update was developed by experts from five medical organizations, led by the Society for Healthcare Epidemiology of America and published in the journal Infection Control and Healthcare Epidemiology. Credit: Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals: 2022 Update, Infection Control & Hospital Epidemiology
Avoiding the unnecessary use of indwelling catheters and promptly removing catheters that are no longer needed are the first steps in preventing catheter-associated urinary tract infections in acute care hospitals, according to new recommendations developed by five medical societies and published today in the journal Infection Control & Hospital Epidemiology.
“Urinary catheters can be associated with infection and also with non-infectious harms like trauma and obstruction,” said Payal Patel, M.D., an infectious disease physician at Intermountain Health and lead author of “Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals: 2022 Update.”
“Prevention of infection related to use of typical indwelling urinary catheters is multidisciplinary. Many members of the health care team, including doctors and nurses, have a role,” continued Dr. Patel.
Urinary tract infections are one of the most common health care-associated infections, and up to three-quarters of urinary tract infections are caused by an indwelling urinary catheter. Catheter-related infections have been associated with higher hospital mortality and increased length of stay at a cost of nearly $2,000 per hospitalized patient.
The updated recommendations include a model, “Disrupting the Lifecycle of the Urinary Catheter,” which identifies alternatives to indwelling catheters, shows how to follow guidance for safely inserting and maintaining catheters, and prompts health care personnel to initiate timely removal. Non-catheter strategies include prompt toileting, urinals, bedside commodes, incontinence garments, and/or the use of non-indwelling catheter strategies such as intermittent straight catheterization or external urinary catheters.
Since duration of catheterization is the most important risk factor for developing infection, the authors recommend at least daily review of continued catheterization, which can include automated reminders of the presence of a catheter or review during rounds of all patients with urinary catheters.
Other essential practices include ensuring supplies are readily available for non-catheter and catheter management of patients’ urinary issues, and ensuring when catheters are used, they are positioned to beds and wheelchairs in ways that avoid kinking of tubing, which increases the risk of infection. Educating health care professionals about urine culture stewardship while providing indications for urine cultures is another new essential practice.
The document updates “Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals,” published in 2014.
The urinary catheter paper is the final installment in the latest Compendium update, which began with publication of strategies to prevent ventilator and non-ventilator associated pneumonia in May of 2022.
More information: Strategies to Prevent Catheter-Associated Urinary Tract Infections in Acute Care Hospitals: 2022 Update, Infection Control (2023).
Provided by Society for Healthcare Epidemiology of America

Leave a Reply