August 9, 2024
by Carmen Rotte, Max Planck Society
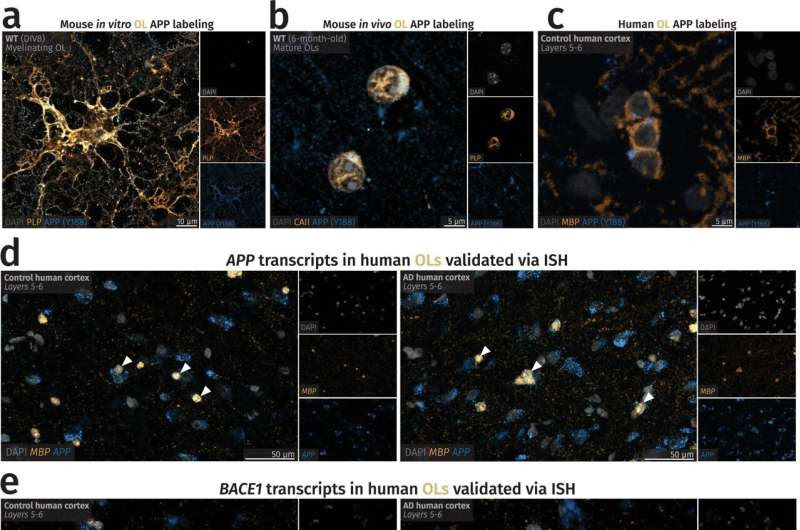
Oligodendrocytes exhibit protein expression of amyloid precursor protein (APP) and an abundance of APP and BACE1 transcripts. Credit: Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01730-3
Memory loss, confusion, speech problems—Alzheimer’s disease is the most common cause of dementia, affecting about 35 million people worldwide, and the number is growing.
The protein amyloid beta, which occurs naturally in the brain, plays a central role in the disease: It accumulates in patients in insoluble clumps that form plaques between neurons in the brain, damaging them.
Researchers at the Max Planck Institute (MPI) for Multidisciplinary Sciences have now shown that, in addition to neurons, special glial cells in the brain also produce amyloid beta. This finding, published in Nature Neuroscience, could open up new avenues for future therapies.
There is no cure for Alzheimer’s disease. However, there are therapeutic approaches to reduce the amyloid plaques in the brain. That can slow down the progression of the disease, but it cannot reverse or stop it.
“Until now, neurons were thought to be the main producers of amyloid beta and have been the main target for new drugs,” explains Klaus-Armin Nave, Director at the MPI for Multidisciplinary Sciences. Results from his Department of Neurogenetics have now shown: In addition to neurons, special glial cells—called oligodendrocytes—play an important role in plaque formation.
“One of the tasks of oligodendrocytes is to form myelin—an insulating layer—and wrap it around the nerve fibers to speed up signal transmission,” explains Andrew Octavian Sasmita, one of the first authors of the study and a former Ph.D. student on Nave’s team.
In a previous study, the Göttingen researchers had already discovered that defective myelin of oligodendrocytes exacerbates Alzheimer’s disease. Do glial cells play an even greater role in the disease than previously thought?
“We have now shown that although neurons are the main producers of amyloid beta, oligodendrocytes also produce a significant amount of the protein which is incorporated into plaques,” says Sasmita. A research group led by Marc Aurel Busche of the University College London (England) recently came to similar conclusions.
Preventing plaque formation
The cells of the nervous system produce amyloid beta by cleaving a larger precursor molecule with the help of an enzyme called BACE1. For their experiments, the researchers specifically knocked out BACE1 in the neurons and oligodendrocytes of mice. They then used 3D light-sheet microscopy to study plaque formation throughout the brain, providing a complete picture of amyloid plaques in all brain regions.
“Oligodendrocytes lacking BACE1 developed about 30% fewer plaques. Knocking out the BACE1 gene in neurons reduced plaque formation by over 95%,” says Constanze Depp, also a first author of the study and a former Ph.D. student in Nave’s department. “Plaque deposits only form when a certain amount of neuronal amyloid beta is present. The oligodendrocytes then contribute to these plaques.”
This threshold could be useful for Alzheimer’s therapies. “If we can successfully inhibit BACE1 before this threshold is reached, the plaques might form later,” Nave emphasizes. That could help to slow down the progression of Alzheimer’s disease at an early stage.
More information: Andrew Octavian Sasmita et al, Oligodendrocytes produce amyloid-β and contribute to plaque formation alongside neurons in Alzheimer’s disease model mice, Nature Neuroscience (2024). DOI: 10.1038/s41593-024-01730-3
Journal information: Nature Neuroscience
Provided by Max Planck Society

Leave a Reply