September 6, 2024
by Karolinska Institutet
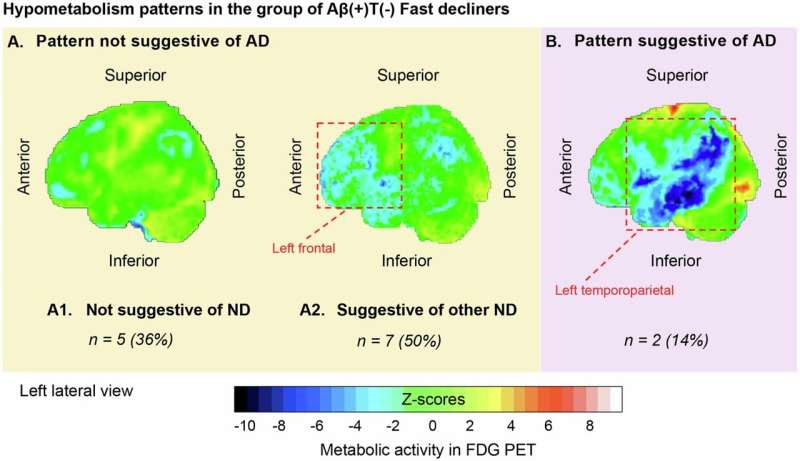
Hypometabolism FDG PET patterns in the group of Aβ(+)T(-) fast decliners (14 out of 19 individuals had available FDG PET scans). Credit: Molecular Psychiatry (2024). DOI: 10.1038/s41380-024-02672-9
A study from Karolinska Institutet, published in the journal Molecular Psychiatry, offers new insights into the progression of Alzheimer’s disease (AD). The research reveals critical differences in the progression of memory loss based on the presence of specific proteins in the brain.
Alzheimer’s disease is the most common form of dementia, characterized by the accumulation of amyloid-beta (Aβ) and tau proteins in the brain, leading to cognitive decline. Traditionally, memory clinics have relied on positron emission tomography (PET) to detect Aβ accumulation. However, recent advances now allow for the detection of tau protein accumulation as well.
The study highlights that individuals with symptoms of memory loss and high levels of tau protein (tau positivity) also exhibit high levels of Aβ (Aβ positivity). This combination is associated with a malignant progression of memory loss due to AD. However, individuals who are Aβ positive but tau negative may experience a more benign progression of symptoms.
“If an individual is positive for Aβ but negative for tau, then the progression of symptoms is likely to be benign. If the symptoms are malignant, it is possible that the cause is not exclusively AD but may also involve other medical conditions that contribute to memory loss. If both Aβ and tau are absent, the cause of memory loss is likely another medical condition rather than AD,” explains Konstantinos Ioannou, Ph.D. student at the Department of Neurobiology, Care Sciences and Society.
This distinction is crucial for accurate diagnosis and treatment planning.
The presence of high levels of tau protein is strongly linked to cognitive decline due to AD. For individuals with high Aβ levels but low tau levels, memory loss may result from multiple medical conditions. In the era of emerging drugs that can remove Aβ, identifying the primary cause of memory loss is essential for determining the most effective treatment for each patient.
“Developing biomarker panels that measure multiple proteins simultaneously will help us understand the complexity of each patient,” says Ioannou, first author of the study. “This approach will allow for more personalized management, tailored to the prognosis or treatment of other contributing factors.”
The research team used PET to measure Aβ and tau protein levels, as well as brain function, in both healthy individuals and patients. Statistical modeling was then applied to evaluate memory loss progression across all participants. Finally, the medical histories of patients with varying levels of tau protein were compared.
Looking ahead, the researchers plan to measure Aβ and tau levels in cerebrospinal fluid and blood samples. This could potentially allow for easier clinical testing to identify individuals for whom AD is the primary cause of memory loss. Additional studies, including MRI scans and brain data from deceased individuals, are also planned to confirm these findings before introducing tau protein measurement into clinical practice.
This study marks a significant step forward in understanding Alzheimer’s disease and improving patient care through more precise diagnostic tools and personalized treatment plans.
More information: Konstantinos Ioannou et al, Tau PET positivity predicts clinically relevant cognitive decline driven by Alzheimer’s disease compared to comorbid cases; proof of concept in the ADNI study, Molecular Psychiatry (2024). DOI: 10.1038/s41380-024-02672-9
Journal information: Molecular Psychiatry
Provided by Karolinska Institutet

Leave a Reply