by Xia & He Publishing Inc.
Credit: Journal of Clinical and Translational Hepatology (2024). DOI: 10.14218/JCTH.2023.00207
Nonalcoholic fatty liver disease (NAFLD), now reclassified as metabolic dysfunction-associated steatotic liver disease (MASLD), and its more severe form, nonalcoholic steatohepatitis (NASH), renamed metabolic dysfunction-associated steatohepatitis (MASH), are increasingly recognized as major contributors to chronic liver disease (CLD) and cirrhosis. These conditions are largely attributed to the epidemic of obesity and type 2 diabetes mellitus in Western populations. As MASLD progresses, it can culminate in serious liver complications, including cirrhosis and hepatocellular carcinoma (HCC).
Sarcopenia, characterized by the loss of muscle mass, strength, and function, is a prevalent yet frequently overlooked complication in patients with CLD. The European Working Group on Sarcopenia in Older People (EWGSOP) defines sarcopenia as a syndrome that involves the progressive and generalized loss of skeletal muscle mass and strength, leading to adverse outcomes such as physical disability, poor quality of life, and death.
In cirrhotic patients, particularly those with decompensated cirrhosis, the prevalence of sarcopenia is alarmingly high, ranging from 30% to 70%. This condition significantly impacts the quality of life, increases morbidity, and elevates mortality rates.
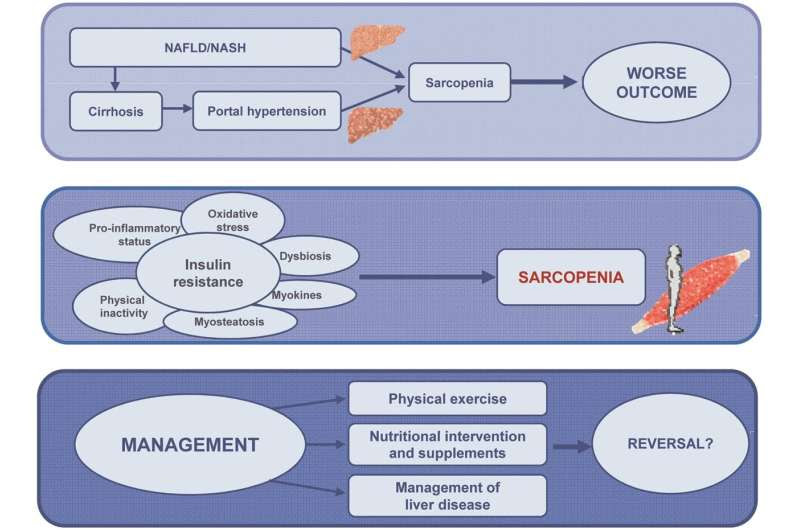
The interplay between sarcopenia and MASLD/NASH is complex and multifaceted. Both conditions share common pathophysiological mechanisms, including chronic inflammation, insulin resistance, and alterations in the liver-muscle-adipose tissue axis. The co-occurrence of sarcopenia and MASLD/NASH exacerbates the progression of liver disease and worsens patient outcomes.
The development of sarcopenia in the context of MASLD is driven by multiple interconnected mechanisms. Chronic liver disease leads to systemic inflammation and hormonal imbalances, which in turn promote muscle protein breakdown and inhibit muscle protein synthesis. Insulin resistance, commonly seen in MASLD, further contributes to muscle catabolism. Additionally, patients with MASLD often exhibit reduced physical activity and poor nutritional status, both of which are critical factors in maintaining muscle mass and function.
Furthermore, myosteatosis, or the infiltration of fat into muscle tissue, is a common feature in patients with MASLD. Myosteatosis not only impairs muscle function but also exacerbates insulin resistance, creating a vicious cycle that accelerates the loss of muscle mass and strength.
Currently, there is no standardized treatment protocol for sarcopenia in patients with MASLD-related cirrhosis due to the paucity of targeted clinical trials. However, several strategies have been proposed to address this dual burden. The cornerstone of managing sarcopenia involves a combination of nutritional interventions and physical exercise.
Nutritional interventions: Ensuring adequate protein intake is crucial for muscle maintenance and growth. Dietary recommendations often include high-protein diets, oral nutritional supplements, and in some cases, specialized formulas designed to address the specific needs of sarcopenic patients. Micronutrient supplementation, particularly with vitamin D and omega-3 fatty acids, has also shown potential benefits in improving muscle function and reducing inflammation.
Physical exercise: Resistance training is the most effective form of exercise for increasing muscle mass and strength. Exercise programs tailored to the individual’s capabilities and limitations can significantly improve physical performance and quality of life. Aerobic exercises, although less effective for muscle hypertrophy, are beneficial for cardiovascular health and should be included as part of a comprehensive exercise regimen.
Pharmacological approaches: Emerging therapies, such as myostatin inhibitors and selective androgen receptor modulators (SARMs), are being investigated for their potential to enhance muscle mass and strength in sarcopenic patients. These pharmacological agents, however, require further validation through rigorous clinical trials before they can be routinely recommended.
The increasing prevalence of MASLD and its complications, including sarcopenia, highlights the urgent need for a deeper understanding and more effective management strategies for these interconnected conditions. Recognizing sarcopenia as a significant determinant of liver disease outcomes necessitates a multidisciplinary approach that integrates nutritional support, tailored exercise programs, and, where appropriate, pharmacological interventions.
Future research should focus on developing and validating specific guidelines for the management of sarcopenia in patients with MASLD-related cirrhosis. Such guidelines would facilitate early identification, comprehensive assessment, and targeted treatment of sarcopenia, ultimately improving the prognosis and quality of life for these patients.
This review emphasizes the importance of addressing sarcopenia as a modifiable risk factor in the management of MASLD-related cirrhosis and advocates for a holistic approach to patient care that encompasses both liver health and muscle integrity. The work is published in the Journal of Clinical and Translational Hepatology.

Leave a Reply