by Claudia Caruana and Ruth Douglas, SciDev.Net
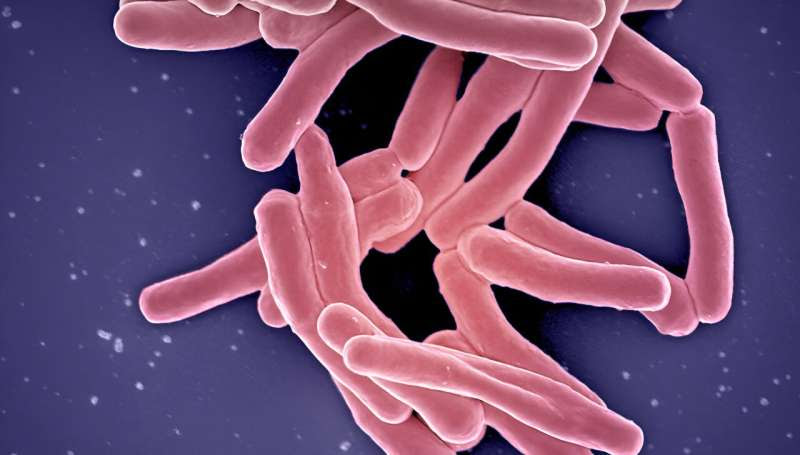
More funding is needed to combat Koch’s bacillus, the bacteria responsible for tuberculosis. Credit: NIAID, ( CC BY 2.0 )
Taking a common antibiotic could more than half the risk of children becoming sick with multidrug resistant tuberculosis (MDR-TB), according to findings presented this week at a conference on lung health.
It is one of a number of emerging breakthroughs in the prevention of TB, which kills about 240,000 children each year—the majority of them aged under 5.
A single, daily dose of levofloxacin reduced the risk of MDR-TB disease in children by 56%, researchers from the Desmond Tutu TB Center at South Africa’s Stellenbosch University announced at the Union Conference on Lung Health in Paris on Thursday (16 November).
Children are particularly vulnerable to MDR-TB, a form of the disease that has developed resistance to two or more of the first-line drugs used against it.
Because of this resistance, treatment of the disease can be a long and difficult process, which many patients don’t complete. In contrast, this preventative drug comes in the form of a child-friendly, fruit-flavored tablet, according to the research funder Unitaid.
An estimated 2 million children a year become newly infected with MDR-TB, which, if left untreated, can develop into what is known as “active TB,” a serious and highly contagious illness that commonly affects the lungs.
“Once it progresses to active disease, multidrug-resistant TB treatment is long and harrowing for children and their families to endure,” said Anneke Hesseling, director of the Desmond Tutu TB Center and principal investigator of the TB-CHAMP trial, at South Africa’s Stellenbosch University.
“This research provides high-quality evidence to cut that risk in half.” By avoiding lengthy treatments, the intervention could also bring cost savings for national health systems, she added.
The late-stage trial involved 1,000 healthy children who had been exposed to MDR-TB in communities with high burdens of TB and MDR-TB across South Africa.
The conference also heard how a separate human trial had found three new, all-oral, shortened regimens for MDR-TB were safe and effective across all populations, including children, pregnant women and people with other illnesses such as HIV.
The endTB clinical trial found the regimens could reduce treatment time by up to two-thirds compared with conventional treatments, which can last up to two years.
Winnie Byanyima, executive director of UNAIDS, said only about 2 in 5 people with drug resistant TB accessed appropriate treatment in 2022, “so it’s great to see these advances in the treatment and prevention of multi-drug resistant TB.”
Finger-prick test
Late last month researchers announced what they said could be a game changer in detecting TB in children, in the form of a simple, rapid analytical tool.
A major reason for the high death toll from TB is the difficulty and delays in diagnosing the disease in children. Most TB tests for adults and children rely on using sputum or phlegm. But small children cannot produce sputum on request. Also, childhood TB has a low bacterial load and non-specific symptoms, often contributing to misdiagnosis or failure to diagnose at an early stage.
The new diagnostic tool requires only a finger prick of blood.
The study, published in The Lancet Infectious Diseases, was led by the Ludwig Maximilian University (LMU) in Munich, Germany, in collaboration with partners from South Africa, Mozambique, Tanzania, Malawi and India.
Laura Olbrich, a medical researcher from LMU and one of the study’s authors, said once diagnosed, 95% of TB cases can be cured.
“So, a test that works on fingerstick blood and can be used without much lab infrastructure could change the problem substantially,” Olbrich said.
The tool, developed in partnership with U.S. diagnostics company Cepheid and currently at prototype stage, identified almost 60% of children with tuberculosis, with 90% specificity, or accuracy.
“This makes the test comparable with or better than all other tests that work with biomarkers [a biological measure used to detect features of disease],” Olbrich added.
According to pediatric specialist Norbert Heinrich, a co-author of the study, the test has the advantage that the blood sample can be conveniently taken from the fingertip and the results are rapid. “We have the results in just over an hour,” he told SciDev.Net. “For most other tests, the samples must be sent to outside laboratories for analysis.”
“This study is an important step forward toward easier methods to detect TB in children,” said Jacqueline Achkar, a professor of medicine, microbiology, and immunology at the Albert Einstein College of Medicine and an infectious disease physician at Motefiore Medical Center, New York.
“Sputum can be hard to obtain from children…therefore, other tests with body fluids that are easy to obtain are urgently needed,” she told SciDev.Net.
WHO roadmap
On Tuesday (14 November), the World Health Organization (WHO) launched the third edition of its Roadmap towards ending TB in children and adolescents, which sets out a five-year plan to improve prevention, treatment and care of childhood TB.
By 2027, 90% of the estimated number of people with TB should be reached with diagnosis and treatment services, while 90% of people at high risk of developing TB should be able to access preventive treatment, under the plan.
According to the WHO, TB is the world’s second deadliest disease next to COVID-19, killing 1.3 million in 2022. It is the leading killer among people with HIV.
An estimated 10.6 million people fell ill with TB in 2022, up from 10.3 million in 2021. Most of these were from Asia Pacific and Sub-Saharan Africa.
The WHO says that progress has been insufficient to meet global TB targets set in 2018, stymied by the pandemic and ongoing conflicts.
More information: Toyin Omotayo Togun et al, Diagnostics for childhood tuberculosis: a marathon rather than a sprint, The Lancet Infectious Diseases (2023). DOI: 10.1016/S1473-3099(23)00517-0
Journal information: Lancet Infectious Diseases
Provided by SciDev.Net

Leave a Reply