by American Society of Hematology
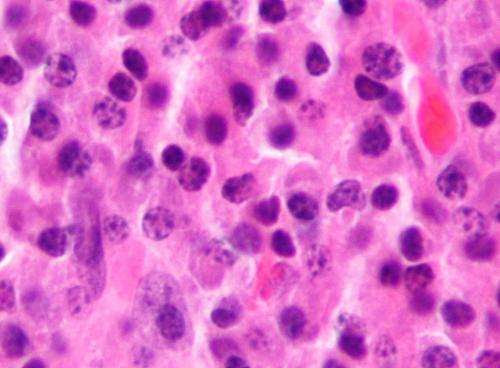
Micrograph of a plasmacytoma, the histologic correlate of multiple myeloma. H&E stain. Credit: Wikipedia/CC BY-SA 3.0
Patients with multiple myeloma treated with idecabtagene vicleucel, known as “ide-cel,” a chimeric antigen receptor (CAR) T-cell therapy, had no difference in overall survival outcomes regardless of race and ethnicity, according to a study published in Blood Advances.
“With this study, we see that Black and white patients with multiple myeloma both respond well to ide-cel,” explained Laura Peres, Ph.D., an epidemiologist at Moffit Cancer Center and the study’s lead author. “We hope that these findings encourage the use of ide-cel in all patients with multiple myeloma.”
Multiple myeloma, a cancer of the plasma cells in the bone marrow, is the second most common blood cancer in the United States, with a five-year survival rate of 56%. Among Black and Hispanic populations, it is the most common blood cancer. While several treatments exist, the condition remains incurable, and most patients who achieve remission eventually relapse.
In CAR T-cell therapies, a patient’s T-cells are removed from their blood and a gene for a receptor that binds to a specific protein on cancer cells is added to help them find and destroy cancer cells. Then, the modified cells are infused back into the patient.
In 2021, ide-cel became the first CAR T-cell therapy to gain approval from the U.S. Food and Drug Administration (FDA) to treat relapsed/refractory (RR) multiple myeloma, a version of the blood cancer that did not respond to treatment or that returned after treatment.
“Non-Hispanic Black individuals are twice as likely to develop multiple myeloma compared to their white counterparts,” emphasized Dr. Peres. “We also know that Black patients are less likely to receive these novel CAR-T therapies and are less represented in clinical trials. So, with this study, we wanted to look at how outcomes differ between racial and ethnic groups.”
To conduct this study, Dr. Peres and her research team collected data from 207 patients at 11 institutions that participated in the U.S. Multiple Myeloma Immunotherapy Consortium. A total of 149 or 72% of patients identified as non-Hispanic white, 30, or 17% identified as non-Hispanic Black, while 22, or 11% identified as Hispanic. Patients with RR multiple myeloma received ide-cel and researchers monitored their remission rates, overall survival, and the prevalence of complications associated with CAR T-cells, following up with patients around nine months after treatment.
Dr. Peres’ findings suggest that non-Hispanic Black patients were more likely to develop cytokine release syndrome—a potentially dangerous side effect of the therapy that causes inflammation—than Hispanic and non-Hispanic white patients (97% vs. 77% vs. 85% respectively). However, the team did not find any significant differences in one’s likelihood of developing severe complications when comparing outcomes by race and ethnicity.
Similarly, they found no significant differences in the incidence of intensive care unit admission, one’s likelihood of reaching complete remission, or overall survival between Black and white patients.
While the overall response rate—the percentage of patients that achieve a partial, very good partial, or complete response to CAR T—was lower among Hispanic patients compared to non-Hispanic Black and white patients, researchers suspect this could, in part, be attributed to the limited number of Hispanic patients included in the study.
Due to the FDA’s approval of ide-cel in March 2021, this study had a limited sample size and follow-up duration. The study was retrospective, and race and ethnicity were self-reported. Conducted across 11 medical institutions, there might be variations in the assessment and management of CAR T-cell associated toxicities.
“These results highlight the need for diverse patient cohorts in research and clinical trials,” said Dr. Peres. “Clinical trials often lack diversity for many reasons such as recruitment barriers, financial considerations, medical mistrust, and cultural insensitivity. But stringent trial eligibility criteria also often exclude racial and ethnic minorities.
“In fact, 75% of our study population would not have been eligible for the trial that led to FDA approval of ide-cel. A lack of clinical trial representation can limit underrepresented groups’ access to life-saving care.”
More information: Laura Peres et al, Blood Advances (2023).
Journal information: Blood Advances
Provided by American Society of Hematology

Leave a Reply