Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention
Zunyou Wu, MD, PhD1; Jennifer M. McGoogan, PhD1
Author Affiliations Article Information
JAMA. Published online February 24, 2020. doi:10.1001/jama.2020.2648
The Chinese Center for Disease Control and Prevention recently published the largest case series to date of coronavirus disease 2019 (COVID-19) in mainland China (72 314 cases, updated through February 11, 2020).1 This Viewpoint summarizes key findings from this report and discusses emerging understanding of and lessons from the COVID-19 epidemic.
Epidemiologic Characteristics of the COVID-19 Outbreak
Among a total of 72 314 case records (Box), 44 672 were classified as confirmed cases of COVID-19 (62%; diagnosis based on positive viral nucleic acid test result on throat swab samples), 16 186 as suspected cases (22%; diagnosis based on symptoms and exposures only, no test was performed because testing capacity is insufficient to meet current needs), 10 567 as clinically diagnosed cases (15%; this designation is being used in Hubei Province only; in these cases, no test was performed but diagnosis was made based on symptoms, exposures, and presence of lung imaging features consistent with coronavirus pneumonia), and 889 as asymptomatic cases (1%; diagnosis by positive viral nucleic acid test result but lacking typical symptoms including fever, dry cough, and fatigue).1
Box.
Key Findings From the Chinese Center for Disease Control and Prevention Report
72 314 Cases (as of February 11, 2020)
Confirmed cases: 44 672 (62%)
Suspected cases: 16 186 (22%)
Diagnosed cases: 10 567 (15%)
Asymptomatic cases: 889 (1%)
Age distribution (N = 44 672)
≥80 years: 3% (1408 cases)
30-79 years: 87% (38 680 cases)
20-29 years: 8% (3619 cases)
10-19 years: 1% (549 cases)
<10 years: 1% (416 cases)
Spectrum of disease (N = 44 415)
Mild: 81% (36 160 cases)
Severe: 14% (6168 cases)
Critical: 5% (2087 cases)
Case-fatality rate
2.3% (1023 of 44 672 confirmed cases)
14.8% in patients aged ≥80 years (208 of 1408)
8.0% in patients aged 70-79 years (312 of 3918)
49.0% in critical cases (1023 of 2087)
Health care personnel infected
3.8% (1716 of 44 672)
63% in Wuhan (1080 of 1716)
14.8% cases classified as severe or critical (247 of 1668)
5 deaths
Most case patients were 30 to 79 years of age (87%), 1% were aged 9 years or younger, 1% were aged 10 to 19 years, and 3% were age 80 years or older. Most cases were diagnosed in Hubei Province (75%) and most reported Wuhan-related exposures (86%; ie, Wuhan resident or visitor or close contact with Wuhan resident or visitor). Most cases were classified as mild (81%; ie, nonpneumonia and mild pneumonia). However, 14% were severe (ie, dyspnea, respiratory frequency ≥30/min, blood oxygen saturation ≤93%, partial pressure of arterial oxygen to fraction of inspired oxygen ratio <300, and/or lung infiltrates >50% within 24 to 48 hours), and 5% were critical (ie, respiratory failure, septic shock, and/or multiple organ dysfunction or failure) (Box).1
The overall case-fatality rate (CFR) was 2.3% (1023 deaths among 44 672 confirmed cases). No deaths occurred in the group aged 9 years and younger, but cases in those aged 70 to 79 years had an 8.0% CFR and cases in those aged 80 years and older had a 14.8% CFR. No deaths were reported among mild and severe cases. The CFR was 49.0% among critical cases. CFR was elevated among those with preexisting comorbid conditions—10.5% for cardiovascular disease, 7.3% for diabetes, 6.3% for chronic respiratory disease, 6.0% for hypertension, and 5.6% for cancer. Among the 44 672 cases, a total of 1716 were health workers (3.8%), 1080 of whom were in Wuhan (63%). Overall, 14.8% of confirmed cases among health workers were classified as severe or critical and 5 deaths were observed.1
COVID-19 rapidly spread from a single city to the entire country in just 30 days. The sheer speed of both the geographical expansion and the sudden increase in numbers of cases surprised and quickly overwhelmed health and public health services in China, particularly in Wuhan City and Hubei Province. Epidemic curves reflect what may be a mixed outbreak pattern, with early cases suggestive of a continuous common source, potentially zoonotic spillover at Huanan Seafood Wholesale Market, and later cases suggestive of a propagated source as the virus began to be transmitted from person to person (Figure 1).1
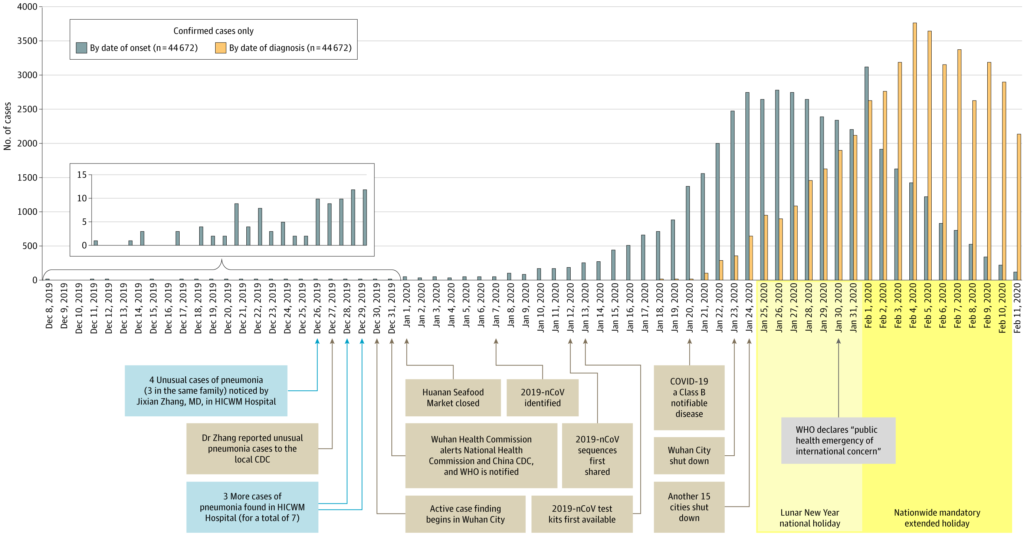
Epidemic Curve of the Confirmed Cases of Coronavirus Disease 2019 (COVID-19)
Daily numbers of confirmed cases are plotted by date of onset of symptoms (blue) and by date of diagnosis (orange). Because, on retrospective investigation, so few cases experienced illness in December, these cases are shown in the inset. The difference between the cases by date of symptom onset curve (blue) and the cases by date of diagnosis curve (orange) illustrates lag time between the start of illness and diagnosis of COVID-19 by viral nucleic acid testing. The graph’s x-axis (dates from December 8, 2019, to February 11, 2020) is also used as a timeline of major milestones in the epidemic response. The first few cases of pneumonia of unknown etiology are shown in blue boxes on December 26 (n = 4) and 28-29 (n = 3). Most other cases that experienced onset of symptoms in December were only discovered when retrospectively investigated. Major epidemic response actions taken by the Chinese government are shown in brown boxes. The normally scheduled Lunar New Year national holiday is shown in light yellow, whereas the extended holiday during which attendance at school and work was prohibited (except for critical personnel such as health workers and police) is shown in dark yellow. This figure was adapted with permission.1 CDC indicates Chinese Center for Disease Control and Prevention; HICWM, Hubei Integrated Chinese and Western Medicine; 2019-nCoV, 2019 novel coronavirus; WHO, World Health Organization.
Comparison of COVID-19 With SARS and MERS
The current COVID-19 outbreak is both similar and different to the prior severe acute respiratory syndrome (SARS; 2002-2003) and Middle East respiratory syndrome (MERS; 2012-ongoing) outbreaks. SARS was initiated by zoonotic transmission of a novel coronavirus (likely from bats via palm civets) in markets in Guangdong Province, China. MERS was also traced to zoonotic transmission of a novel coronavirus (likely from bats via dromedary camels) in Saudi Arabia. All 3 viral infections commonly present with fever and cough, which frequently lead to lower respiratory tract disease with poor clinical outcomes associated with older age and underlying health conditions. Confirmation of infection requires nucleic acid testing of respiratory tract samples (eg, throat swabs), but clinical diagnosis may be made based on symptoms, exposures, and chest imaging. Supportive care for patients is typically the standard protocol because no specific effective antiviral therapies have been identified.
The World Health Organization (WHO) declared the SARS outbreak contained on July 5, 2003. A total of 8096 SARS cases and 774 deaths across 29 countries were reported for an overall CFR of 9.6%. MERS is still not contained and is thus far responsible for 2494 confirmed cases and 858 deaths across 27 countries for a CFR of 34.4%. Despite much higher CFRs for SARS and MERS, COVID-19 has led to more total deaths due to the large number of cases. As of the end of February 18, 2020, China has reported 72 528 confirmed cases (98.9% of the global total) and 1870 deaths (99.8% of the global total). This translates to a current crude CFR of 2.6%. However, the total number of COVID-19 cases is likely higher due to inherent difficulties in identifying and counting mild and asymptomatic cases. Furthermore, the still-insufficient testing capacity for COVID-19 in China means that many suspected and clinically diagnosed cases are not yet counted in the denominator.2 This uncertainty in the CFR may be reflected by the important difference between the CFR in Hubei (2.9%) compared with outside Hubei (0.4%).1,2 Nevertheless, all CFRs still need to be interpreted with caution and more research is required.
Most secondary transmission of SARS and MERS occurred in the hospital setting. Transmission of COVID-19 is occurring in this context as well—3019 cases have been observed among health workers as of February 11, 2020 (of whom there have been 1716 confirmed cases and 5 deaths).1 However, this is not a major means of COVID-19 spread. Rather, it appears that considerable transmission is occurring among close contacts. To date, 20 provinces outside of Hubei have reported 1183 case clusters, 88% of which contained 2 to 4 confirmed cases. Of note, 64% of clusters documented thus far have been within familial households (Chinese Center for Disease Control and Prevention presentation made to the WHO Assessment Team on February 16, 2020). Thus, although COVID-19 seems to be more transmissible than SARS and MERS, and many estimates of the COVID-19 reproductive number (R0) have already been published, it is still too soon to develop an accurate R0 estimate or to assess the dynamics of transmission. More research is needed in this area as well.
Response to the COVID-19 Epidemic
Since 2003, the Chinese government has improved its epidemic response capacity. Some of these efforts are evident in the response to COVID-19 (Figure 2). For example, in the 2002-2003 SARS outbreak, 300 cases and 5 deaths already had occurred by the time China reported the outbreak to the WHO, whereas in the COVID-19 outbreak, only 27 cases and zero deaths had occurred when the WHO was notified (January 3, 2020) (Figure 2). From the time of WHO notification, 2 months elapsed before SARS-CoV was identified compared with only 1 week from the time of WHO notification until 2019-nCoV was identified.
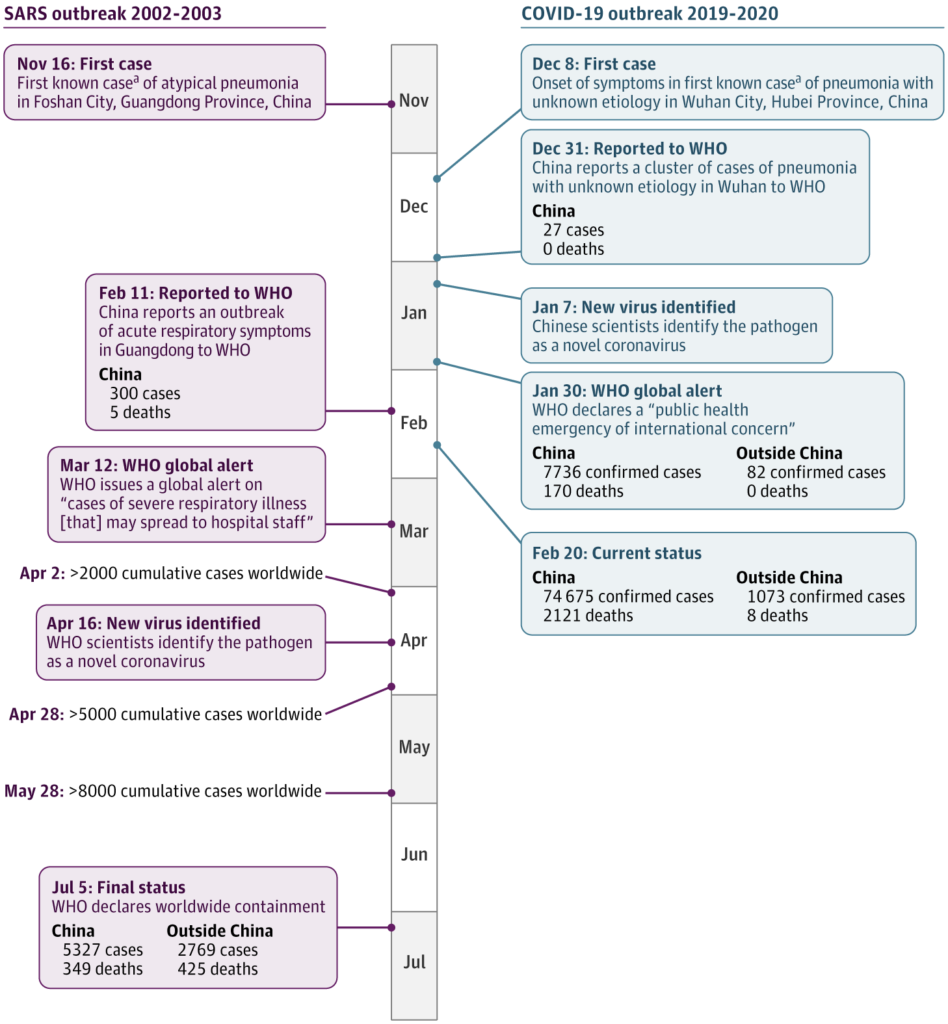
Timeline Comparing the Severe Acute Respiratory Syndrome (SARS) and Coronavirus Disease 2019 (COVID-19) Outbreaks
The timeline of events for the SARS outbreak (left) from first case to final worldwide containment. The timeline of events for the COVID-19 outbreak (right) from the onset of symptoms for the first case on December 8, 2019, to status on February 20, 2020. Over the course of the first 2 months, more than 70 000 cases have been confirmed and many more are suspected. WHO indicates World Health Organization.
aIdentified later retrospectively.
The timing of the COVID-19 outbreak, prior to China’s annual Lunar New Year holiday, was an important factor as China considered how to respond to the outbreak. Culturally, this is the largest and most important holiday of the year. It is the expectation that people return to their family homes, which is the cause for the several billion person-trips made by residents and visitors during this time, mostly on crowded planes, trains, and buses. Knowing this meant each infected person could have numerous close contacts over a protracted time and across long distances, the government needed to quickly act. However, it was not only the speed of the government’s response, but also the magnitude of that response that were influenced by the impending holiday travel time. Knowing that specific treatment and prevention options, such as targeted antiviral drugs and vaccines, were not yet available for COVID-19, China focused on traditional public health outbreak response tactics—isolation, quarantine, social distancing, and community containment.3-5
Identified case patients with COVID-19 were immediately isolated in designated wards in existing hospitals, and 2 new hospitals were rapidly built to isolate and care for the increasing numbers of cases in Wuhan and Hubei. People who had been in contact with COVID-19 cases were asked to quarantine themselves at home or were taken to special quarantine facilities, where they could be monitored for onset of symptoms. Enormous numbers of large gatherings were canceled, including all Lunar New Year celebrations, and traffic in Wuhan and in cities across Hubei was restricted and closely monitored. Virtually all transportation was subsequently restricted at a national level. All of these measures were instituted to achieve social distancing. In addition, an estimated 40 million to 60 million residents of Wuhan and 15 other surrounding cities within Hubei Province were subjected to community containment measures. Although these types of traditional outbreak response actions have been successfully used in the past, they have never been executed on such a large scale.
There have been some questions about whether these actions are reasonable and proportional responses to the outbreak. Some have argued that a number of these approaches may infringe on the civil liberties of citizens, and some of these measures have been referred to as “draconian.” However, it is not only individual rights that must be considered. The rights of those who are not infected, but at risk of infection, must be considered as well. Whether these approaches have been effective (eg, in terms of reduced infections and deaths averted), and whether these potential benefits have outweighed the costs (eg, economic losses), will be debated for years.4,5
Next Steps
Importantly, another major goal of China’s current outbreak response activities is to help “buy time” for science to catch up before COVID-19 becomes too widespread. China must now focus on adjusting tactics and strategies as new evidence becomes available.3,6 Much remains to be done and many questions remain unanswered. China is very grateful for the help it is receiving from the international scientific, health, and public health communities. The global society is more interconnected than ever, and emerging pathogens do not respect geopolitical boundaries. Proactive investment in public health infrastructure and capacity is crucial to effectively respond to epidemics like COVID-19, and it is critical to continue to improve international surveillance, cooperation, coordination, and communication about this major outbreak and to be even better prepared to respond to future new public health threats.
Back to topArticle Information
Corresponding Author: Zunyou Wu, MD, PhD, Chinese Center for Disease Control and Prevention, 155 Changbai Rd, Beijing 102206, China ([email protected]).
Published Online: February 24, 2020. doi:10.1001/jama.2020.2648
Conflict of Interest Disclosures: None reported.
Funding/Support: This work was supported by the National Health Commission of the People’s Republic of China (2018ZX10721102).
Role of the Funder/Sponsor: The funder had no role in the preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.
Disclaimer: The opinions expressed herein reflect the collective views of the coauthors and do not necessarily represent the official position of the Chinese Center for Disease Control and Prevention.
Additional Contributions: We thank China CDC Weekly for its permission to re-create the epidemic curve with modifications.
References
1.
Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Weekly. Accessed February 20, 2020. http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51
2.
Battegay M, Kuehl R, Tschudin-Sutter S, Hirsch HH, Widmer AF, Neher RA. 2019-Novel coronavirus (2019-nCoV): estimating the case fatality rate: a word of caution. Swiss Med Wkly. 2020;150:w20203. doi:10.4414/smw.2020.20203PubMedGoogle Scholar
3.
McCloskey B, Heymann DL. SARS to novel coronavirus: old lessons and new lessons. Epidemiol Infect. 2020;148:e22. doi:10.1017/S0950268820000254PubMedGoogle Scholar
4.
Du Z, Wang L, Cauchemez S, et al. Risk for transportation of 2019 novel coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis. 2020;26(5). doi:10.3201/eid2605.200146Google Scholar
5.
Wilder-Smith A, Freedman DO. Isolation, quarantine, social distancing and community containment: pivotal role for old-style public health measures in the novel coronavirus (2019-nCoV) outbreak. J Travel Med. 2020;taaa020. doi:10.1093/jtm/taaa020PubMedGoogle Scholar
6.
Cowling BJ, Leung GM. Epidemiological research priorities for public health control of the ongoing global novel coronavirus (2019-nCoV) outbreak. Euro Surveill. 2020;25(6). doi:10.2807/1560-7917.ES.2020.25.6.2000110PubMedGoogle Scholar

Leave a Reply