August 29, 2024
by Juntendo University Research Promotion Center
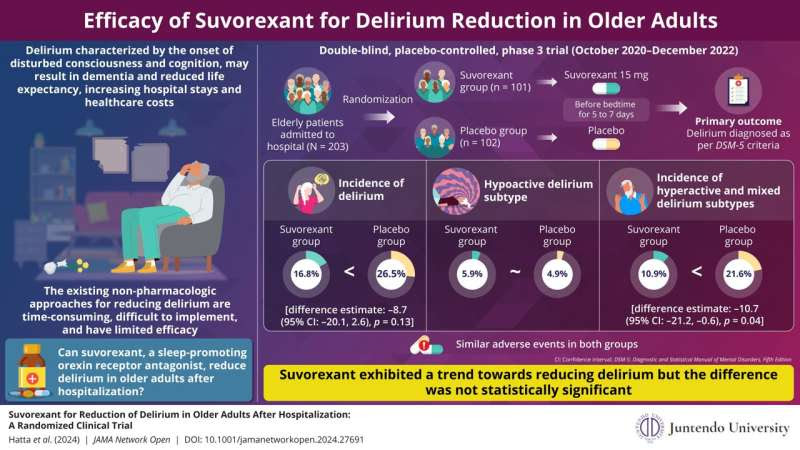
Delirium increases the risks of falls and dementia among older adults and the burden on healthcare providers. Researchers assess whether the sleep-promoting medication suvorexant could reduce delirium in older adults since insomnia is a major risk factor for delirium. Credit: Professor Kotaro Hatta from Juntendo University Nerima Hospital, Japan
Delirium is a sudden onset and temporary state of disturbed consciousness or cognition, occurring due to underlying medical issues like fever or alcohol withdrawal. It is most common among older hospitalized adults aged 75 years or above, leading to increased risk of falls, dementia, low life expectancy, and high health care expenses.
Non-pharmacological approaches to prevent or reduce delirium are time-consuming, hard to implement, and partially effective. So, pharmacological interventions offer hope. Insomnia, a significant risk factor for delirium, could be alleviated with sleep-promoting medications.
However, not all medications are suitable. Some may aggravate delirium. Interestingly, suvorexant (an orexin receptor antagonist) promotes sleep by blocking a neuropeptide called orexin that regulates wakefulness. This mechanism could prevent delirium, as shown by many studies.
Against this backdrop, a team of researchers involving Professor Kotaro Hatta from the Department of Psychiatry at Juntendo University Nerima Hospital in Tokyo, Japan, tested whether suvorexant can reduce delirium in older adults at high risk for delirium after hospitalization.
Their study was published in JAMA Network Open on August 16, 2024.
Reflecting on the motivation behind the study, Prof. Hatta says, “While working as a psychiatric liaison at a general hospital, I was busy managing patients with delirium every day. So, when an orexin receptor antagonist became available, we decided to use this drug to target the sleep-wake cycle disturbances, a primary clinical manifestation of delirium.”
To this end, researchers conducted a double-blind, placebo-controlled, phase 3 randomized clinical trial across 50 Japanese hospitals from October 2020 to December 2022. The trial included 203 Japanese adults aged 65 to 90 years who were at high risk for delirium and hospitalized for sudden illness or scheduled surgery.
Participants were randomly assigned to two groups, with 101 receiving suvorexant (15 mg) and 102 receiving a placebo each night for five to seven days. They were assessed daily for delirium based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition criteria.
Subtypes of delirium—namely hyperactive (marked by agitation, hallucination, and impulsivity), hypoactive (marked by drowsiness and apathy), and mixed (shifts between hyperactive and hypoactive delirium)—were also recorded for those who exhibited delirium. Researchers then compared both groups to assess whether suvorexant made a difference.
Consistent with expectations, suvorexant showed a trend toward reducing delirium, with only 16.8% of participants exhibiting delirium compared to 26.5% in the placebo group. However, the difference was not statistically significant. Both groups also experienced similar adverse events, such as constipation and vomiting.
The incidence of hypoactive delirium was similar between the suvorexant (5.9%) and placebo groups (4.9%). However, in the post-hoc exploratory analysis, the incidence of hyperactive and mixed delirium was lower in the suvorexant group (10.9%) compared to placebo (21.6%). Delirium with a hyperactive component was considered since it interferes with surgery or treatment, making it burdensome for hospital staff.
As the results suggest, suvorexant may not have preventive effects on hypoactive delirium but could benefit hyperactive and mixed delirium.
Explaining the results, Prof. Hatta emphasizes, “The lack of significant reduction of delirium after taking suvorexant was surprising since previous studies reported positive findings. However, these studies did not distinguish between delirium subtypes except for one study that excluded hypoactive delirium due to its irrelevance in postoperative management and another that defined the primary outcome as delirium of any type. So, we believe that previous studies have focused more on hyperactive or mixed delirium and overlooked hypoactive delirium.”
Prof. Hatta says, “Addressing this issue can increase the life expectancy of older adults and reduce the burden on health care providers.”
More information: Kotaro Hatta et al, Suvorexant for Reduction of Delirium in Older Adults After Hospitalization, JAMA Network Open (2024). DOI: 10.1001/jamanetworkopen.2024.27691
Journal information: JAMA Network Open
Provided by Juntendo University Research Promotion Center

Leave a Reply