by Bob Yirka , Medical Xpress
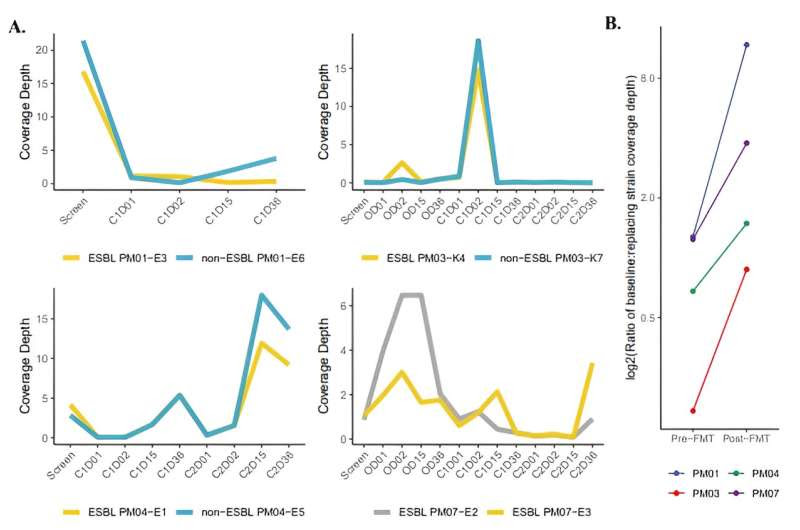
Depth of coverage of metagenome reads from participant stool samples mapped to representative genomes from participants with detected conspecific strain replacement after FMT. (A) Depth of coverage for patients PM01, PM03, PM04, and PM07 show higher coverage depth for replacing strains after FMT. (B) Ratio of coverage depth for baseline to replacing conspecific strains increases after FMT. Participant stool metagenome reads were mapped to baseline and replacing strain genomes and coverage depth estimates from inStrain were used to calculate a log2-transformed ratio comparing screening visit to last visit where both strains were detected (PM01—C1D36, PM03—C1D02, PM04—C2D36, PM07—C2D36). Credit: Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abo2750
A team of infectious disease researchers at the Emory University School of Medicine, working with colleagues from the Georgia Institute of Technology, has found via clinical trial that fecal transplants after kidney transplantation reduce the susceptibility of patients to infections by multi-drug-resistant organisms (MDROs).
In their study, reported in the journal Science Translational Medicine, the group tested the impact of fecal microbiota transfer (FMT) on kidney transplant patients receiving care at Emory Transplant Center, in Atlanta.
Prior research has shown that people who receive kidney transplantation are at risk of developing an infection from MDROs. This is because patients are given antibiotics to prevent general infections, killing all non-drug-resistant organisms. The absence of competing organisms allows MDROs to flourish, putting these patients at serious risk. In this new effort, the researchers tested giving kidney transplant patients FMTs as a way to reduce the risk of MDRO infections.
The test was conducted in the form of a phase I clinical trial involving 11 patients who underwent kidney transplants. In addition to a new kidney, each patient also received an FMT via enema. Stool samples were tested every day for 36 days following their surgery. The research team notes that they chose the enema method of FMT for the trial because it has the lowest chance of introducing undesired organisms to the gut biota. The researchers also gave some of the patients a second FMT if they continued to show high levels of MDROs.
The researchers found significant results in most of the patients—eight of the patients who had contracted an MDRO infection tested negative for it after 36 days. The research team also conducted a genetic analysis of stool samples from the patients in the trial and found evidence of reduced numbers of MDROs. They conclude that the FMT procedure works because it forces MDROs to compete for resources inside the gut biome.
More information: Michael H. Woodworth et al, Fecal microbiota transplantation promotes reduction of antimicrobial resistance by strain replacement, Science Translational Medicine (2023). DOI: 10.1126/scitranslmed.abo2750
Journal information: Science Translational Medicine
© 2023 Science X Network

Leave a Reply