by Baker Heart & Diabetes Institute
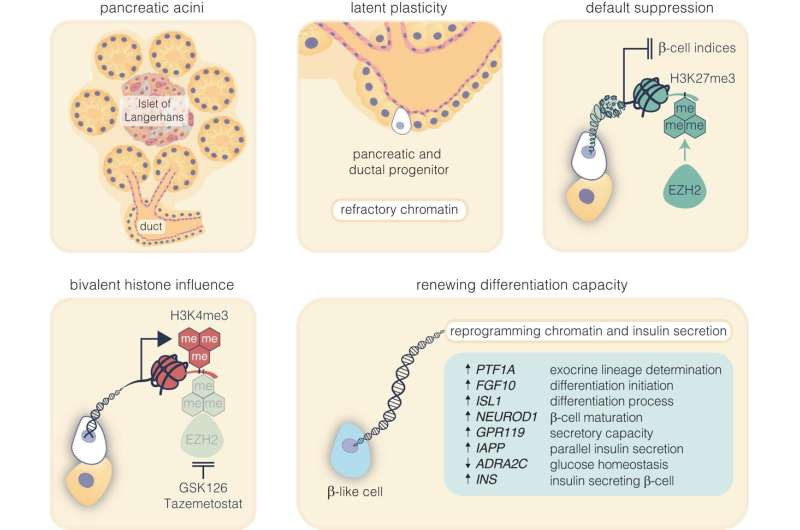
Pharmacological inhibition of EZH2 catalyzes pancreatic progenitor activation and β-cell maturation. The schematic outlines the progression from pancreatic multipotent progenitors to mature insulin-secreting β-cells, highlighting the regulatory target of EZH2 inhibitors, GSK126 and Tazemetostat. Credit: Signal Transduction and Targeted Therapy (2024). DOI: 10.1038/s41392-023-01707-x
Researchers are zeroing in on the ultimate quest to regenerate insulin in pancreatic stem cells and replace the need for regular insulin injections.
Baker Heart and Diabetes Institute researchers have demonstrated in an article published in Signal Transduction and Targeted Therapy that newly made insulin cells can respond to glucose and produce insulin following stimulation with two U.S. Food and Drug Administration-approved drugs in as little as 48 hours.
Further, they confirmed this pathway of awakening the insulin-producing cells is viable in age groups from 7 to 61, providing much-needed insights into the mechanisms underlying the regeneration of beta cells.
Using pancreatic cells derived from a child and adult type 1 diabetic donors, and from a non-diabetic person, a team led by Professor Sam El-Osta demonstrated how insulin-producing cells that are destroyed in people with type 1 diabetes can be regenerated into glucose sensing and functionally secreting insulin cells.
In this latest study by the Human Epigenetics team, they show small molecule inhibitors that are currently used for rare cancers and approved by the U.S. FDA can rapidly return insulin production in pancreatic cells destroyed by diabetes.
While current pharmaceutical options for diabetes treatment help control blood glucose levels they do not prevent, stop or reverse the destruction of insulin-secreting cells.
The novel therapeutic approach holds the potential to become the first disease modifying treatment for type 1 diabetes by facilitating glucose responsive insulin production by harnessing the patient’s remaining pancreatic cells, thereby enabling people living with diabetes to potentially achieve independence from round-the-clock insulin injections.
This disease-modifying treatment also represents a promising solution for the significant number of Australians living with insulin dependent diabetes, who account for 30% of those with type 2 diabetes.
The development of novel pharmacological therapies aimed at restoring pancreas function addresses the stark reality of donor organ shortages.
“We consider this regenerative approach an important advance towards clinical development,” Professor El-Osta said. “Until now, the regenerative process has been incidental, and lacking confirmation, more importantly the epigenetic mechanisms that govern such regeneration in humans remain poorly understood,” he said.
This research shows that 48 hours of stimulation with small molecule inhibitors is sufficient to restore insulin production from damaged pancreatic cells.
JDRF Senior Research Fellow, Dr. Keith Al-Hasani said the next step was to investigate the novel regenerative approach in a preclinical model. The aim is to develop these inhibitors as drugs to restore insulin production in people living with diabetes.
As the work progresses, so too does the need to translate rapidly. More than 530 million adults are living with diabetes, with that number expected to rise to 643 million by 2030.
More information: Keith Al-Hasani et al, EZH2 inhibitors promote β-like cell regeneration in young and adult type 1 diabetes donors, Signal Transduction and Targeted Therapy (2024). DOI: 10.1038/s41392-023-01707-x
Provided by Baker Heart & Diabetes Institute

Leave a Reply