by Massachusetts General Hospital
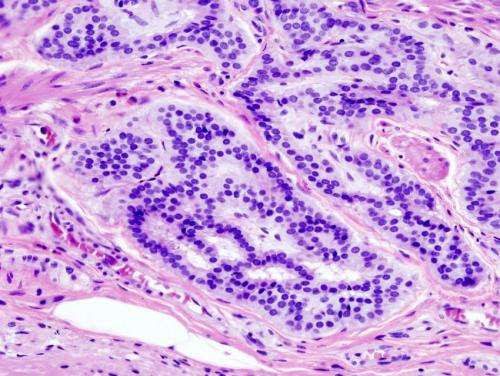
Cancer — Histopathologic image of colonic carcinoid. Credit: Wikipedia/CC BY-SA 3.0
Screening for colorectal cancer—the second most common cause of cancer-related death in the United States—can save lives by detecting both pre-cancerous lesions that can be removed during the screening procedure, and colorectal cancer in its early stages, when it is highly curable.
Screening is most commonly performed with endoscopy: visualization of the entire colon and rectum using a long flexible optical tube (colonoscopy), or of the lower part of the colon and rectum with a shorter flexible tube (sigmoidoscopy).
This week, the United States Preventive Services Task Force (USPSTF) lowered the recommended beginning age for screening from 50 to 45 for persons without a family history of colorectal cancer. However, its recommendation to continue periodically until age 75, after which the decision to undergo screening can be based on an individual’s health and risk factors, remains unchanged.
Yet there has been very little hard evidence to support or contradict the recommendation to stop routine screening at age 75—until now. As researchers from Massachusetts General Hospital (MGH) report in JAMA Oncology, screening endoscopy for persons older than 75 in otherwise good health can reduce the risk of colorectal cancer incidence and cancer-related death by approximately 40%.
The researchers also found, however, that screening did not provide a significant survival benefit for individuals older than 75 with cardiovascular disease, diabetes or three or more other health conditions.
“Until now, there really weren’t clear data to help us decide whether patients should be screened after age 75,” says co-investigator Andrew T. Chan. MD, MPH, a gastroenterologist and chief of the Clinical and Translational Epidemiology Unit at MGH. “Current guidance was largely based on modeling and extrapolation of studies conducted in other age groups, and not on solid data to show whether screening was actually helpful in an older population.”
To answer this important question, Chan and colleagues looked at data on the incidence of colorectal cancer and colorectal cancer-related deaths among participants in two large U.S. health studies: the Nurses’ Health Study and the Health Professionals Follow-up Study. In both, participants fill out biannual questionnaires on demographics, lifestyle factors, screening, medical history and disease outcomes.
For the current study, the investigators examined data on participants who were followed from 1988 through 2016, focusing on the history of screening sigmoidoscopy or colonoscopy in 56,374 who reached 75 years of age during study follow-up.
The researchers identified 661 cases of colorectal cancer and 323 colorectal cancer-related deaths after age 75.
They found that screening after age 75 was associated with a 39% decrease in colorectal cancer incidence and a 40% decrease in risk of death related to colorectal cancer, regardless of whether participants had been screened before age 75.
Among participants who had undergone screening before 75 years of age, screening after age 75 was associated with a 33% reduction in colorectal cancer incidence and a 42% decrease in colorectal cancer-related death compared with those who were not screened after reaching 75.
Similarly, for participants who were screened for the first time only after age 75, the respective declines in incidence and death were 49% and 37% compared with those who were never screened.
In contrast, participants with cardiovascular disease or multiple co-morbidities did not benefit from screening after 75.
“These are the first empirical data that really demonstrate that there is value in continuing screening past age 75 for many individuals. But the key take-home message is that screening should be tailored according to individual risk factors,” says Chan.

Leave a Reply