Research begins to pick apart the mechanisms behind a deadly COVID-19 complication.
Purple rashes, swollen legs, clogged catheters and sudden death — blood clots, large and small, are a frequent complication of COVID-19, and researchers are just beginning to untangle why. For weeks, reports have poured in of the disease’s effects throughout the body, many of which are caused by clots. “This is like a storm of blood clots,” says Behnood Bikdeli, a fourth-year cardiology fellow at Columbia University in New York City. Anyone with a severe illness is at risk of developing clots, but hospitalized patients with COVID-19 appear to be more susceptible.
Studies from the Netherlands and France suggest that clots appear in 20% to 30% of critically ill COVID-19 patients1,2. Scientists have a few plausible hypotheses to explain the phenomenon, and they are just beginning to launch studies aimed at gaining mechanistic insights. But with the death toll rising, they are also scrambling to test clot-curbing medications.
Double whammy
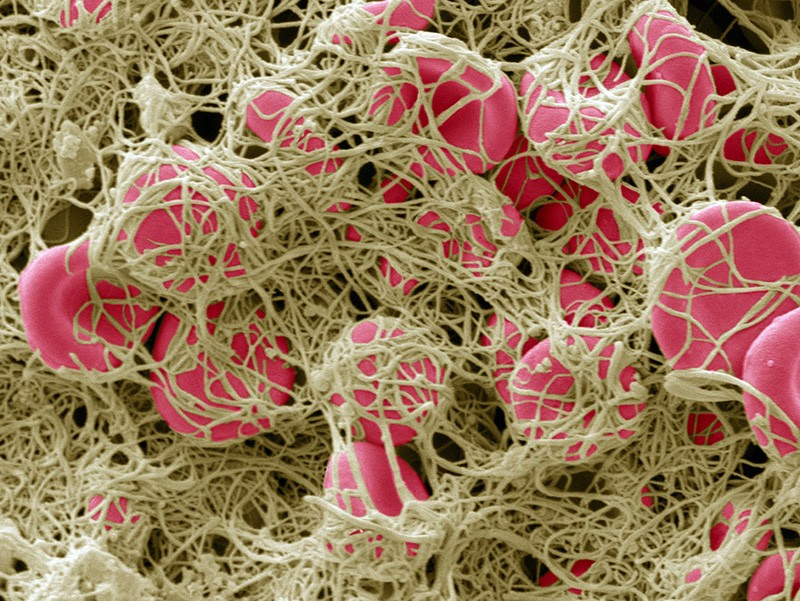
Blood clots, jelly-like clumps of cells and proteins, are the body’s mechanism to stop bleeding. Some researchers view clotting as a key feature of COVID-19. But it’s not just their presence that has scientists puzzled: it’s how they show up. “There are so many things about the presentations that are a little bit unusual,” says James O’Donnell, director of the Irish Centre for Vascular Biology at the Royal College of Surgeons in Dublin.
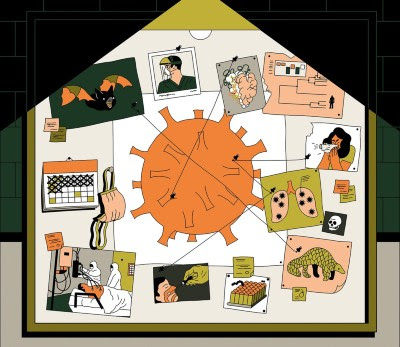
Profile of a killer: the complex biology powering the coronavirus pandemic
Blood thinners don’t reliably prevent clotting in people with COVID-19, and young people are dying of strokes caused by the blockages in the brain. And many people in hospital have drastically elevated levels of a protein fragment called D-dimer, which is generated when a clot dissolves. High levels of D-dimer appear to be a powerful predictor of mortality in hospitalized patients infected with coronavirus3.
Researchers have also observed miniature clots in the body’s smallest vessels. Jeffrey Laurence, a haematologist at Weill Cornell Medicine in New York City, and his colleagues examined lung and skin samples from three people infected with COVID-19 and found that the capillaries were clogged with clots4. Other groups, including a team led by O’Donnell, have reported similar findings5.
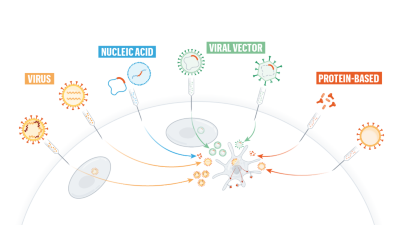
The race for coronavirus vaccines: a graphical guide
“This is not what you’d expect to see in someone who just has a severe infection,” he says. “This is really very new.” This might help to explain why some people have critically low blood-oxygen readings, and why mechanical ventilation often doesn’t help. It’s a “double hit”, says O’Donnell. Pneumonia clogs the tiny sacs in the lungs with fluid or pus, and microclots restrict oxygenated blood from moving through them.
Viral impacts
Why this clotting occurs is still a mystery. One possibility is that SARS-CoV-2 is directly attacking the endothelial cells that line the blood vessels. Endothelial cells harbour the same ACE2 receptor that the virus uses to enter lung cells. And there is evidence that endothelial cells can become infected: researchers from the University Hospital Zurich in Switzerland and Brigham and Women’s Hospital in Boston, Massachusetts, observed SARS-Cov-2 in endothelial cells inside kidney tissue6. In healthy individuals, the blood vessel is “a very smoothly lined pipe”, says Peter Liu, chief scientific officer at the University of Ottawa Heart Institute. The lining actively stops clots from forming. But viral infection can damage these cells, prompting them to churn out proteins that trigger the process.
The virus’s effects on the immune system could also affect clotting. In some people, COVID-19 prompts immune cells to release a torrent of chemical signals that ramps up inflammation, which is linked to coagulation and clotting through a variety of pathways. And the virus appears to activate the complement system, a defence mechanism that sparks clotting. Laurence’s group found that small, clogged vessels in lung and skin tissue from people with COVID-19 were studded with complement proteins. All these systems — complement, inflammation, coagulation — are interrelated, says Agnes Lee, director of the Hematology Research Program at the University of British Columbia in Vancouver, Canada. “In some patients with COVID, all of those systems are kind of in hyperdrive.”

How does COVID-19 kill? Uncertainty is hampering doctors’ ability to choose treatments
But Lee adds that there could be other factors at play that aren’t specific to COVID-19. People with the disease who become hospitalized typically have a number of risk factors for clotting. They might be elderly or overweight, and could have high blood pressure or diabetes. They show up with high fevers and, because they’re seriously ill, have probably been immobilized. They might have a genetic predisposition to clotting, or be taking medications that increase the risk. “It’s kind of like a perfect storm,” she says.
Race to new therapies
Even as researchers begin to unravel how clotting occurs in people with COVID-19, they’re sprinting to test new therapies aimed at preventing and busting clots. Blood-thinning medications are standard of care for patients in the intensive-care unit, and those with COVID-19 are no exception. But dosing is a matter of hot debate. “The question is now, how aggressive should you be?” says Robert Flaumenhaft, chief of the division of homeostasis and thrombosis at Beth Israel Deaconess Medical Center in New York City. Researchers from Mount Sinai School of Medicine, also in New York City, reported that hospitalized patients with COVID-19 on mechanical ventilation who received blood thinners had a lower mortality than those who weren’t treated with them. But the team couldn’t rule out other explanations for the observation, and high doses of these drugs carry risks7.
At Columbia University in New York City, researchers are launching a clinical trial to compare the standard clot-preventing doses of blood thinners with a higher dose in people who are critically ill with COVID-19. Similar trials are planned for Canada and Switzerland. And scientists at Beth Israel Deaconess Medical Center have begun enrolment for a clinical trial to evaluate an even more powerful clot-busting medication called tissue plasminogen activator, or tPA. This drug is more potent, but carries higher risks of serious bleeding than do blood thinners.

Hopes rise for coronavirus drug remdesivir
Scientists hope that these trials and others will provide the data necessary to help physicians to make difficult treatment decisions. Lee worries about the amount of ‘reactionary medicine’ happening. “People are changing their therapeutic approach in reaction to their local and personal experience,” she says. She understands the impetus, “but we have to remember the main thing is first do no harm”.

Leave a Reply