Heidi Ledford
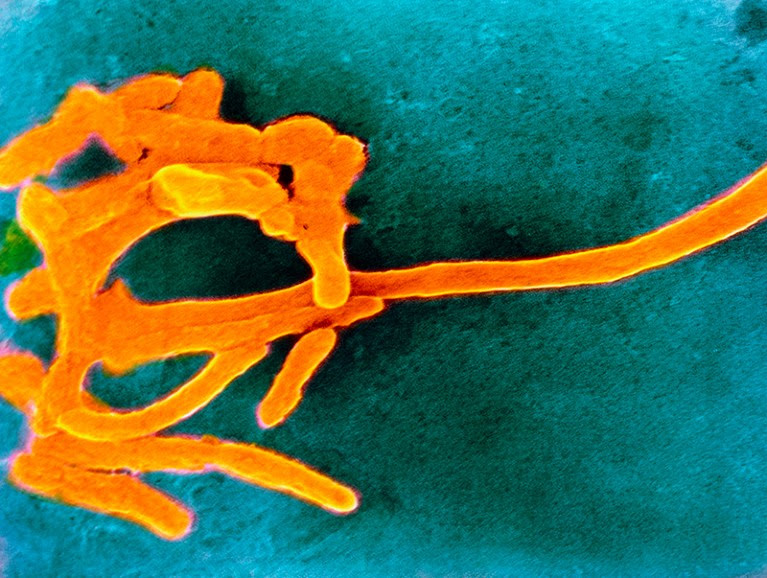
Fusobacterium has been linked with endometriosis. Credit: CNRI/SPL
Infection by a particular group of bacteria could be linked to endometriosis, a painful condition that affects up to 10% of women and girls of reproductive age.
In a study of 155 women in Japan, members of the bacterial genus Fusobacterium were found in the uteruses of around 64% of those with endometriosis, and 7% of those who do not have the condition1. Follow-up experiments in mice infected with Fusobacterium showed that treatment with an antibiotic could reduce the size and frequency of the lesions, which are associated with endometriosis.
Researchers will need to do more work before the findings, published on 14 June in Science Translational Medicine, can be used to develop treatments for endometriosis, says Elise Courtois, a genomicist who studies the disease at the Jackson Laboratory in Farmington, Connecticut.
But the results highlight growing interest in the potential role of microbes in endometriosis, which has limited treatment options and whose origins are poorly understood. “There are definitely things that make us suspect the microbiome is implicated in endometriosis,” says Courtois. “Genetics doesn’t explain everything.”
Painful lesions
Endometriosis is caused by the migration of tissue from the lining of the uterus, called the endometrium, to other parts of the body — most often to organs in the pelvic region — where it attaches and grows. It often causes lesions on reproductive organs and is associated with reduced fertility. Furthermore, people with lesions on their ovaries have an increased risk of developing ovarian cancer.
The most common symptom of endometriosis is pain, which can be severe. Treatments include hormone therapies, which also act as contraceptives, and surgery to remove the lesions. “We want to find new therapies,” says Yutaka Kondo, a cancer biologist at Nagoya University in Japan and a co-author of the paper. “But first we have to know the reason why people suffer from endometriosis.”
Kondo and his colleagues analysed endometrial tissue from women with and without the condition. They found that samples from those with endometriosis were more likely to host bacteria belonging to the genus Fusobacterium. Fusobacterium were often found in the mouth, gut and vagina, and have been linked to other conditions, such as gum disease.
To see whether Fusobacterium could affect the course of endometriosis directly, the team transplanted endometrial tissue from one set of mice into the abdominal cavity of another. Within weeks, endometriotic lesions formed in the recipient mice. Using this model, the researchers found that lesions tended to be more abundant and larger in mice that had also been inoculated with Fusobacterium than in those that hadn’t. Treating the mice with the antibiotics metronidazole or chloramphenicol, administered vaginally, reduced the development of endometriosis, and shrank the number and size of the lesions.
A clinical trial in women with endometriosis is now under way to find out whether antibiotics could relieve some of their symptoms, says Kondo.
Missing pieces
The results are compelling, but the story is still missing a few key pieces, says Courtois. For example, it would be useful to test the association between Fusobacterium and endometriosis in a more diverse population, she says. Courtois and others have successfully lobbied the Connecticut state government to set up a repository of endometrial samples for research that will include tissue from an ethnically diverse population, as well as transgender and gender diverse people. (This article uses ‘women’ to describe people who are at risk for endometriosis, while recognizing that not all people who identify as women have a uterus, and not all people who have a uterus identify as women.)
More extensive research in people is particularly important because mice — which do not menstruate or form spontaneous endometrial lesions — are limited as models of the condition. Kondo’s mouse study focused on lesions that form on the ovaries, whereas in people, lesions can also form elsewhere in the body, including in the colon and bladder. “These are really intriguing results and potentially exciting,” says Krina Zondervan, head of the Nuffield Women’s and Reproductive Health department at the University of Oxford, UK. “But we’re really at the infancy of this.”

Leave a Reply