JUNE 19, 2024
by UT Southwestern Medical Center
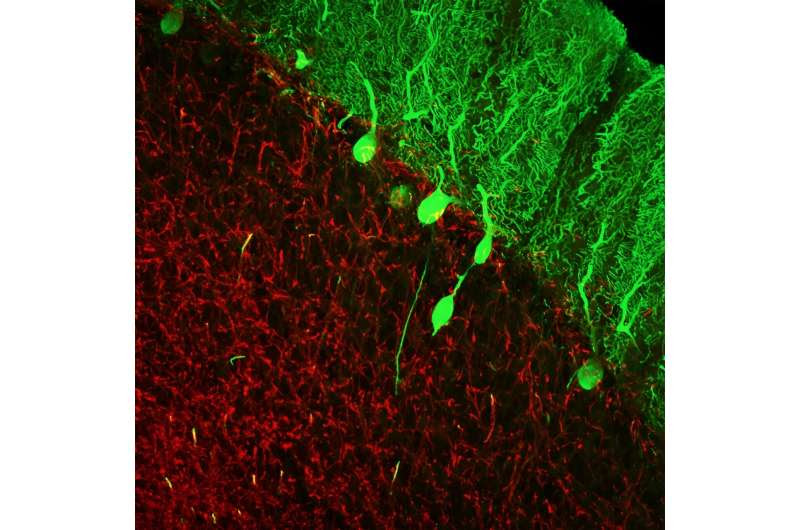
Changes in the brains of patients with essential tremor are centered on a group of neurons in the cerebellum known as Purkinje cells, the round and oval green objects in this image. Credit: Annals of Clinical and Translational Neurology (2024). DOI: 10.1002/acn3.52068
A statistical tool designed to analyze 11 characteristics of postmortem brains reliably diagnosed a common neurodegenerative disease known as essential tremor (ET), a study led by researchers at UT Southwestern Medical Center and Columbia University shows.
Their findings, 20 years in the making and published in the Annals of Clinical and Translational Neurology, could eventually help relatives of deceased ET patients know their hereditary risk of getting the disease.
“These results are exciting because they show that these markers of pathology, when taken as a whole, can really distinguish brains with this disease from a normal brain,” said Elan Louis, M.D., M.S., Chair and Professor of Neurology at UT Southwestern and an Investigator in the Peter O’Donnell Jr. Brain Institute.
Dr. Louis co-led the study with longtime collaborator Phyllis Faust, M.D., Ph.D., Professor of Pathology and Cell Biology at Columbia University Vagelos College of Physicians and Surgeons.
ET is the second-most common neurodegenerative disease worldwide, affecting about 7 million people in the U.S. and producing about 1,000 diagnoses every day, Dr. Louis explained.
Marked by rhythmic trembling of the hands, head, and/or other body areas and often accompanied by nonmotor symptoms such as anxiety, depression, and sleep difficulties, ET shares features with several other neurodegenerative diseases, including Parkinson’s and Alzheimer’s.
But unlike those conditions, which can be definitively diagnosed after death by analyzing microscopic sections of brains, ET can only be diagnosed clinically through a neurological history and examination of living patients. Some estimates suggest ET is misdiagnosed in 30% to 50% of cases, Dr. Louis said.
Because first-degree relatives of ET patients (such as a parent, sibling, or child) are nearly five times more likely to develop the disease than the general population, having a way to definitively diagnose it—even after death—would be useful. However, few studies have assessed metrics that differ between the brains of healthy individuals and those with ET, a necessary step toward making accurate postmortem diagnoses.
Two decades ago, Dr. Louis began addressing this problem by establishing the Essential Tremor Centralized Brain Repository at Columbia University—a collection of ET patients’ brains that now numbers in the hundreds.
By carefully analyzing characteristics of these brains, Dr. Louis, Dr. Faust, and their colleagues have discovered 37 different metrics that can help distinguish ET brains from healthy ones. Although the researchers have studied each of these characteristics in isolation, producing more than 70 peer-reviewed papers, no studies had tested whether a combination of these metrics could reliably tell ET and healthy brains apart.
Homing in on 11 particularly robust metrics, all of which focused on Purkinje cells (a neuron in the cerebellum that’s particularly affected in ET) and neighboring cell populations, Drs. Louis, Faust, and colleagues applied a variety of select statistical methods and developed machine learning algorithms that can provide a positive or negative ET diagnosis to pathologists.
After “training” the algorithms with data from healthy and ET brain sections, the researchers ran the algorithms on data from new brain sections. Their findings showed sensitivity and specificity—measures of accuracy—greater than 90% for the majority of diagnoses delivered by the algorithms.
The researchers have developed a web-based application that pathologists can use to input their own metrics from brain slices for ET diagnoses.
Dr. Louis noted that future research may focus on using artificial intelligence (AI) to provide a visual analysis of brain sections, saving pathologists the work of annotating brain features.
Eventually, he added, findings from this study, which emphasize the importance of Purkinje cells in ET, could be used to develop more neuroimaging-based diagnoses for ET in living patients so they can receive effective treatments, which are currently in development.
More information: Phyllis L. Faust et al, Pathologically based criteria to distinguish essential tremor from controls: analyses of the human cerebellum, Annals of Clinical and Translational Neurology (2024). DOI: 10.1002/acn3.52068

Leave a Reply