Medical University of South Carolina researchers discover cellular process that naturally protects the brain after injury, informing future treatments for brain disease.
MEDICAL UNIVERSITY OF SOUTH CAROLINA
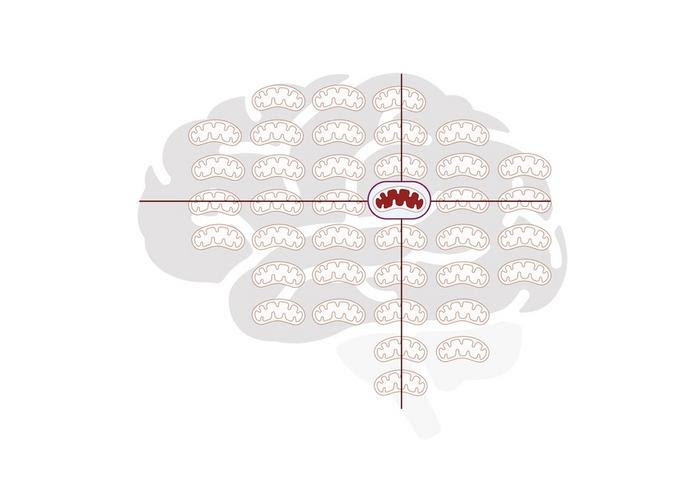
IMAGE:
SCHEMATIC OF BRAIN WITH SUPERIMPOSED MITOCHONDRIA. DR. ONDER ALBAYRAM’S TEAM AT THE MEDICAL UNIVERSITY OF SOUTH CAROLINA FOUND THAT, THANKS TO A NATURAL NEUROPROTECTIVE RESPONSE, DAMAGED MITOCHONDRIA ARE VACUUMED UP AT THE TIME OF BRAIN INJURY AND BEYOND.
CREDIT: MEDICAL UNIVERSITY OF SOUTH CAROLINA; IMAGE COURTESY OF DR. ONDER A’BAYRAM
A team of Medical University of South Carolina researchers, led by Onder Albayram, Ph.D., reports in PNAS Nexus that they have discovered a novel protective response by which the brain naturally repairs itself after traumatic brain injury. Findings could lead to drug treatments that improve the brain’s ability to recover after concussions and prevent long-term brain disease.
“Brain recovery mechanisms are very, very powerful,” said Albayram. “We don’t always have to develop new treatment approaches. We can also just give the brain a chance to heal itself properly.”
Repetitive mild traumatic brain injury, or repeated concussions, are common, especially among athletes in high-contact sports or military personnel involved in combat. The long-term health consequences of a concussion range from mild to severe.
For some people, repeated blows to the head can trigger a domino effect of secondary brain disease. They can develop chronic traumatic encephalopathy, a progressive type of dementia with no known cure. In fact, brain injuries are the No. 1 environmental risk factor for neurodegenerative brain diseases, such as Alzheimer’s disease or other dementias, said Albayram.
“This is the $1 million question: ‘Why do some athletes live healthily into retirement, while others develop brain disease?’” asked Albayram. “We believe it is because the recovery mechanisms in the brain may not be functioning well for some people.”
After concussions, damaged brain tissue builds up in the part of the cellular compartment called the mitochondria, he explained. This accumulation of damaged tissue prevents the mitochondria from functioning well, leading the brain cell to die. To repair itself, the brain can vacuum up the damaged mitochondria in a process called mitophagy.
The protein p17 has been shown to play a small but unique role in mitophagy in other parts of the body. Triggered by stress, the p17 protein transports important enzymes to the cell, flags the damaged tissue and initiates the healing process of mitophagy. Albayram and his team wanted to find out if p17 played a similar protective function in the brain.
This is the first study to show that the protein p17 does indeed play a crucial role in protecting the brain after repeated concussions. When researchers removed p17 in the brain cells of mice, they developed secondary disease after injury.
Albayram and his team then tested a therapeutic approach for secondary brain disease. They created an analog drug that artificially triggered the restorative process of mitophagy in mice. Administering this drug to mice healed most of their brain disease.
To test their findings clinically, Albayram and his team examined postmortem human brains with and without long-term brain disease from concussions. Albayram was surprised to find that protein p17 levels were notably lower in the brains with disease. This outcome confirms what the team discovered in preclinical models – that protein p17 plays a small but mighty role in how the brain protects itself from disease.
Protein p17 could be a target for future treatments that protect the brain after concussions and prevent long-term health consequences.
Because researchers were able to trigger this recovery process in a preclinical model, a future goal is to develop similar drug treatments for humans. Yet, beyond just traumatic brain injury, these findings could inform how we treat brain disease broadly.
Albayram encourages brain scientists not to reinvent the wheel. Just as vaccines boost the natural protective properties of the body to fight viruses, we can improve the recovery properties of the brain to fight disease.
“We can help the brain to cure itself,” said Albayram.
The content in the underlying article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
About the Medical University of South Carolina
Founded in 1824 in Charleston, MUSC is the state’s only comprehensive academic health system, with a unique mission to preserve and optimize human life in South Carolina through education, research and patient care. Each year, MUSC educates more than 3,200 students in six colleges – Dental Medicine, Graduate Studies, Health Professions, Medicine, Nursing and Pharmacy – and trains more than 900 residents and fellows in its health system. MUSC brought in more than $300 million in research funds in fiscal year 2023, leading the state overall in research funding. MUSC also leads the state in federal and National Institutes of Health funding. For information on academic programs, visit musc.edu.
As the health care system of the Medical University of South Carolina, MUSC Health is dedicated to delivering the highest-quality and safest patient care while educating and training generations of outstanding health care providers and leaders to serve the people of South Carolina and beyond. Patient care is provided at 16 hospitals (includes owned or governing interest), with approximately 2,700 beds and four additional hospital locations in development, more than 350 telehealth sites and nearly 750 care locations situated in all regions of South Carolina. In 2023, for the ninth consecutive year, U.S. News & World Report named MUSC Health University Medical Center in Charleston the No. 1 hospital in South Carolina. To learn more about clinical patient services, visit muschealth.org.
MUSC has a total enterprise annual operating budget of $5.9 billion. The nearly 26,000 MUSC family members include world-class faculty, physicians, specialty providers, scientists, students, affiliates and care team members who deliver groundbreaking education, research, and patient care.
JOURNAL
PNAS Nexus
DOI
10.1093/pnasnexus/pgae018
METHOD OF RESEARCH
Experimental study
SUBJECT OF RESEARCH
Human tissue samples
ARTICLE TITLE
p17/C18-ceramide-mediated mitophagy is an endogenous neuroprotective response in preclinical and clinical brain injury
ARTICLE PUBLICATION DATE
7-Feb-2024
COI STATEMENT
The authors declare no competing interest.

Leave a Reply