The results of a large-scale screening study could be used to develop blood tests to diagnose diseases such as Alzheimer’s before symptoms take hold.
By Miryam Naddaf
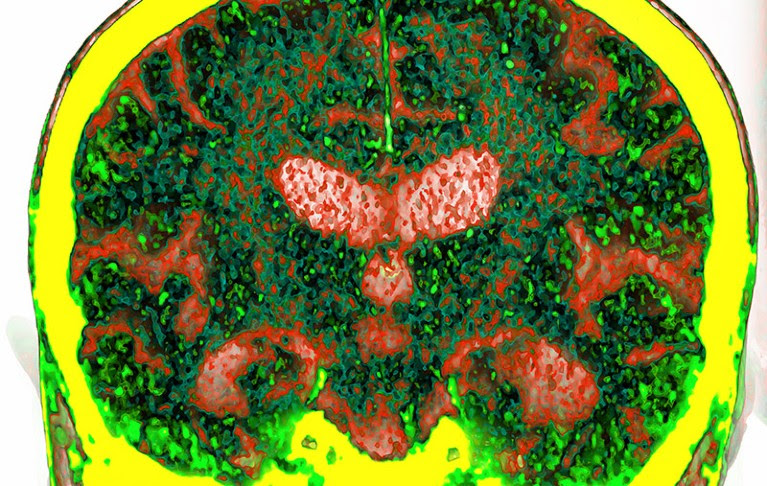
Coloured CT scan of a coronal section through the brain of a patient with Alzheimer’s disease.
A computed-tomography scan of a brain affected by Alzheimer’s disease, the most common cause of dementia.Credit: Vsevolod Zviryk/Science Photo Library
An analysis of around 1,500 blood proteins has identified biomarkers that can be used to predict the risk of developing dementia up to 15 years before diagnosis.
The findings, reported today in Nature Aging1, are a step towards a tool that scientists have been in search of for decades: blood tests that can detect Alzheimer’s disease and other forms of dementia at a very early, pre-symptomatic stage.
Researchers screened blood samples from more than 50,000 healthy adults in the UK Biobank, 1,417 of whom developed dementia in a 14-year period.
They found that high blood levels of four proteins — GFAP, NEFL, GDF15 and LTBP2 — were strongly associated with dementia.
“Studies such as this are required if we are to intervene with disease-modifying therapies at the very earliest stage of dementia,” said Amanda Heslegrave, a neuroscientist at University College London, in a statement to the Science Media Centre in London.
Late diagnosis
According to the World Health Organization, more than 55 million people worldwide currently live with dementia.
People are often diagnosed only when they notice memory problems or other symptoms. At that point, the disease might have been progressing for years. “Once we diagnose it, it’s almost too late,” says study co-author Jian-Feng Feng, a computational biologist at Fudan University in Shanghai, China. “And it’s impossible to reverse it.”
Dementia risk linked to blood-protein imbalance in middle age
By screening 1,463 proteins in blood samples from 52,645 people, the authors found that increased levels of GFAP, NEFL, GDF15 and LTBP2 were associated with dementia and Alzheimer’s disease. For some participants who developed dementia, blood levels of these proteins were outside normal ranges more than ten years before symptom onset.
GFAP, a protein that provides structural support to nerve cells called astrocytes, has already been proposed as a diagnostic marker for Alzheimer’s disease2, as has GDF15.
The latest study finds that people with high levels of GFAP in their blood are more than twice as likely as people with normal levels to develop dementia, and are nearly three times as likely to develop Alzheimer’s.
The authors used machine learning to design predictive algorithms, combining the four protein biomarkers with demographic factors such as age, sex, education level and family history. They trained the model on information from two-thirds of the study participants, and tested its performance using data from the remaining 17,549 people.
The model predicted the incidence of three subtypes of dementia, including Alzheimer’s disease, with about 90% accuracy, using data from more than ten years before participants were officially diagnosed.
The authors say their findings could be used to develop blood tests that identify people at risk of developing dementia. Other researchers caution that the new biomarkers need further validation before being used as clinical screening tools.
The study “needs to be replicated and biomarkers that enable us not only to screen for disease risk but also to differentiate between diseases should be a priority”, said Heslegrave.
doi: https://doi.org/10.1038/d41586-024-00418-9
References
Guo, Y. et al. Nature Aging https://doi.org/10.1038/s43587-023-00565-0 (2024).
Shir, D. et al. Alzheimers Dement. 14, e12291 (2022).

Leave a Reply