WEST VIRGINIA UNIVERSITY
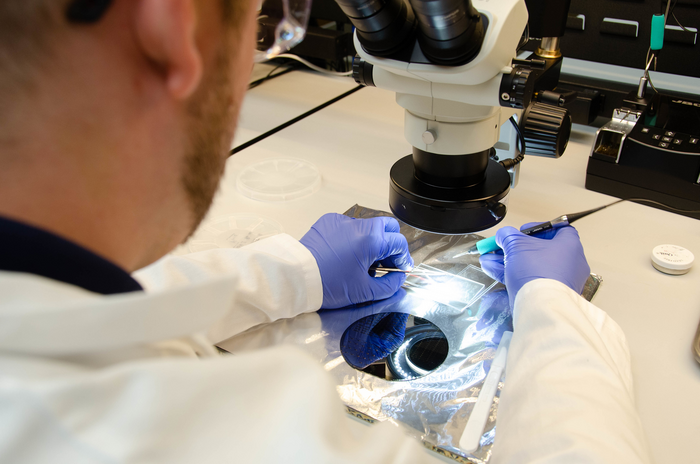
IMAGE: THE MOUSEFLEX ELECTRODE CREATED BY WVU RESEARCHERS WILL ADVANCE TESTING OF VAGUS NERVE STIMULATION, A CUTTING-EDGE BIOELECTRONIC TREATMENT FOR CONDITIONS THAT RANGE FROM EPILEPSY TO ARTHRITIS TO HYPERTENSION. HERE JUSTIN VANKIRK, A DOCTORAL CANDIDATE IN MECHANICAL AND AEROSPACE ENGINEERING, RELEASES MICROFABRICATED MOUSEFLEX ELECTRODES FROM A SILICON WAFER AND SOLDER-INTEGRATES LEADS TO THE DEVICE FOR ELECTROCHEMICAL TESTING.
CREDIT: WVU PHOTO/PAIGE NESBIT
West Virginia University engineers are taking a major step into “bioelectronic medicine,” a cutting-edge approach that uses electric current as a treatment for pain and disease, with the development of MouseFlex. The device will facilitate research into a technique called “vagus nerve stimulation” or VNS.
The vagus nerve is responsible for involuntary body functions such as heart rate, breathing and digestion.
Because VNS trials on mice must happen before new bioelectronic treatments can be tested on humans, the MouseFlex — a tiny electrode that has been formed into a cuff shape, like the cuff of a shirt sleeve — fits around the vagus nerve of a mouse and delivers electrical impulses.
According to its developers, the MouseFlex outperforms existing technology when it comes to withstanding both the electric current flowing through it and the handling it sustains during the course of surgery.
Biomedical engineer Tao Sun, a research assistant professor at the Benjamin M. Statler College of Engineering and Mineral Resources, said the MouseFlex not only enables more effective rodent trials of VNS treatments, but its design could be adapted for humans.
“This research is important because our flexible electrodes remain functional after electrical stimulation,” Sun said. “They achieve intimate contact with the mouse vagus nerve and they tolerate surgical handling. The MouseFlex will immediately benefit neuroscientists and researchers in neural engineering, but patients with drug-resistant disease are the long-distance beneficiaries.”
The study results appear in the journal Acta Biomaterialia.
“Vagus nerve stimulation is used for patients with conditions such as drug-resistant epilepsy,” said Loren Rieth, associate professor in the Department of Mechanical and Aerospace Engineering. “VNS devices treat those conditions by stimulating the left vagus nerve in the neck, adjusting nerve signals that coordinate the function of the body’s organ systems. The vagus nerve links your brain to organs such as the heart, lungs or stomach. The name ‘vagus’ refers to ‘the wanderer,’ as the nerve branches and spreads to connect those organs with your brain.”
Rieth said human vagus nerve branches in the neck “are about a 10th of an inch in diameter and have roughly 100,000 nerve fibers. Cooked spaghetti is a good analogy for the size and ‘softness’ of the vagus nerve in humans, but our research deals with the vagus nerve in mice, which is 20 times smaller: the diameter of a thick strand of hair. The MouseFlex electrodes that fit around that nerve are about 10 times thinner than a human hair.”
Due to the small size of both the mouse vagus nerve and the electrodes, it has been challenging to interface with the nerve and challenging for the electrodes to remain stable throughout the process of electrical stimulation.
Sun said he was surprised by how well the MouseFlex met those challenges.
“Robustness of electrodes on this level is rare and very exciting,” he said. “All MouseFlex electrodes remained functional after one billion cycles of electrical stimulation at eight milliamps — the most aggressive electrical stimulation I’ve seen to date in peer research.
“After we performed the surgery, then removed the electrodes and cleaned them, the electrochemical performance largely reversed to the level it had before the surgery, which means that these electrodes do tolerate surgical handling. That’s quite important for clinical studies and for commercialization.”
Rieth estimated that roughly 125,000 people around the world have VNS stimulators for epilepsy or depression. However, a new condition being evaluated for VNS treatment is rheumatoid arthritis, an autoimmune condition in which the immune system attacks the body’s joints. One company — SetPoint Medical — is conducting a multicenter clinical trial on VNS to treat rheumatoid arthritis, and Dr. Peter Konrad, chair of the WVU School of Medicine Department of Neurosurgery within the Rockefeller Neuroscience Institute, is leading one of the clinical trial sites at Health Sciences.
“If treatment for autoimmune conditions like rheumatoid arthritis works and devices are approved for that purpose, then the number of VNS patients will likely increase significantly,” Rieth predicted, pointing to other widespread medical conditions with the potential to respond to bioelectronic treatment, including reactive airway disease and heart disease.
“VNS systems don’t have major safety concerns,” he said. “The surgery to place the electrode and stimulator does have risks, but neurosurgeons follow well-established procedures. There can be side effects such as voice changes from stimulation, which for epilepsy happens every few minutes, but these rarely require turning off the stimulator. Of course, new treatments might have different safety concerns, and that is a critical part of the Food and Drug Administration’s review process.”
Sun noted several additional conditions for which vagus nerve stimulation using flexible electrodes like the MouseFlex shows promise: depression, obesity and high blood pressure, also known as hypertension.
“For many drug-resistant patients, reliable and safe vagus nerve modulation opens new avenues to effective treatments with few or no side effects,” Sun said. “And our MouseFlex technology could also interface with nerves besides the vagus nerve — the sciatic and sacral nerves and the spinal cord, for example. Stimulating the spinal cord is effective for managing chronic pain and could restore lost motion capability for paralyzed patients.”
Editor’s note: The protocols for the in-vivo study regarding stimulation safety and efficacy of MouseFlex electrodes were approved by the Institutional Animal Care and Use Committee (IACUC) at the Feinstein Institutes for Medical Research (Manhasset, NY, USA). The Feinstein Institutes follow the National Institute of Health (NIH) guidelines for the ethical treatment of animals.

Leave a Reply