by Yale University
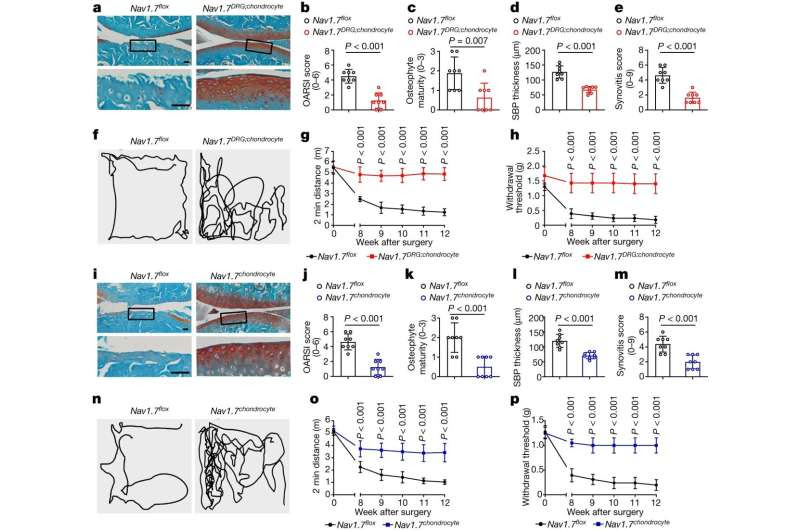
a, Safranin O and Fast Green-stained sections of knee joints of mice with the indicated genotype (n = 8). Scale bar, 50 µm. b–e, OARSI score (b), osteophyte development (c), subchondral bone plate (SBP) thickness (d) and synovitis score (e) in indicated mice 12 weeks after DMM (n = 8). f, Traces of open field testing at 12 weeks after DMM surgery. g,h, Two-minute travel distance (g) and von Frey testing (h) in DMM-operated mice at the indicated time points after surgery (n = 8). i, Safranin O and Fast Green-stained sections of knee joints (n = 8). Scale bars, 50 µm. j–m, OARSI score (j), osteophyte development (k), SBP thickness (l), and synovitis score (m) in indicated mice 12 weeks after DMM surgery (n = 8). n, Traces of open field testing at 12 weeks after DMM surgery. o,p, Two-minute travel distance (o) and von Frey testing (p) in DMM-operated mice at the indicated time points after surgery (n = 8). b–e,j–m, Data are mean ± s.d., P values by two-tailed unpaired Student’s t-test. g,h,o,p, Data are mean ± 95% confidence interval (CI), P values by two-tailed multiple unpaired Student’s t-test with Welch’s correction. Credit: Nature (2024). DOI: 10.1038/s41586-023-06888-7
Yale researchers have identified a drug target that may alleviate joint degeneration associated with osteoarthritis, a debilitating condition that afflicts as many as 30 million people in the United States alone, which they report in the journal Nature.
Pain relievers and lifestyle changes, such as exercise and reduced excess weight, have long been the therapies most commonly used to treat the joint stiffness and pain caused by degenerative disease, but there is a pressing need for therapies that can prevent joint breakdown that occurs in osteoarthritis.
It is known that specialized proteins known as sodium channels found in cell membranes produce electrical impulses in “excitable” cells within muscles, the nervous system, and the heart. In previous research, Yale’s Stephen G. Waxman identified the key role of one particular sodium channel, called Nav1.7, in the transmission of pain signals.
Now, the labs of Chuan-Ju Liu, the Charles W. Ohse Professor of Orthopedics, and Waxman, the Bridget M. Flaherty Professor of Neurology and professor of neuroscience and pharmacology, both at Yale School of Medicine, have found that the same Nav1.7 channels are also present in non-excitable cells that produce collagen and help maintain the joints in the body.
Osteoarthritis, the most common form of arthritis, is a degenerative disease caused by the breakdown of cartilage that eases friction between the joints. It occurs most commonly in the hands, hips, and knees.
In the new study, the researchers deleted Nav1.7 genes from these collagen-producing cells, significantly reducing joint damage in two osteoarthritis models in mice.
They also demonstrated that drugs used to block Nav1.7—including carbamazepine, a sodium channel blocker currently used to treat epilepsy and trigeminal neuralgia—also provided substantial protection from joint damage in the mice.
“The function of sodium channels in non-excitable cells has been a mystery,” Waxman said. “This new study provides a window on how small numbers of sodium channels can powerfully regulate the behavior of non-excitable cells.”
“The findings open new avenues for disease-modifying treatments,” added Wenyu Fu, a research scientist in the Liu laboratory and first author of the study.
More information: Stephen Waxman, Nav1.7 as chondrocyte regulator and therapeutic target for osteoarthritis, Nature (2024). DOI: 10.1038/s41586-023-06888-7. www.nature.com/articles/s41586-023-06888-7
Journal information: Nature
Provided by Yale University

Leave a Reply