by UT Southwestern Medical Center
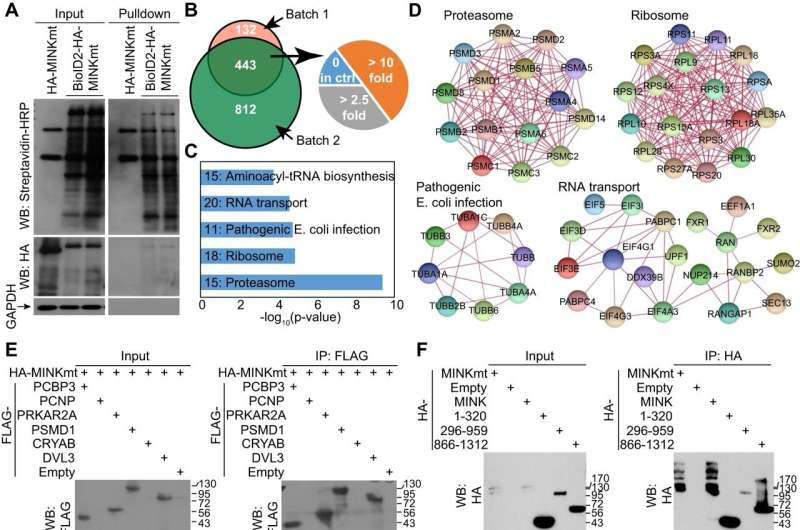
MAP4K interactome and the effect on RANGAP1 subcellular distribution. A Western-blotting analysis of proteins after proximity labeling in ALS1-hiMNs at 10 dpi. B Venn diagram of proteins from two batches of samples analyzed by Mass Spectrometry. With a cutoff of 2.5-fold enrichment, 443 proteins were common to these two sets of data, including proteins with no expression in control group (0 in ctrl), proteins with over 2.5-fold changes, and proteins with over 10-fold changes. C The top 5 KEGG pathways. D STRING analysis of association networks of proteins in the top 4 KEGG pathways. E Validation of protein associations in HEK293T cells by co-immunoprecipitations (co-IP) and western blots. F co-IP assays in HEK293T cells showing association of MINK1mt with RANGAP1 or RAN. G Confocal images showing subcellular distribution of RANGAP1 or RAN in ALS1-hiMNs at 52 dpi. Arrows indicate aggregated cytoplasmic RANGAP1 foci. Scale bar, 10 µm. H MINKmt improves nuclear/cytoplasmic (Nuc/Cyt) ratios of the indicated proteins in ALS1-hiMNs at 52 dpi (mean ± SEM; n = 30 neurons per group; ***p < 0.001, Student’s t-test). I MINKmt improves soma sizes of ALS1-hiMNs at 52 dpi (mean ± SEM; n = 30 neurons per group; ***p < 0.001, Student’s t-test). Credit: Cell Death & Disease (2024). DOI: 10.1038/s41419-023-06395-7
UT Southwestern Medical Center researchers have identified an experimental molecular compound that improved survival among cellular models and mouse models of amyotrophic lateral sclerosis (ALS), the fatal neurodegenerative disease. Their findings, reported in Cell Death & Disease, offer promise for the potential development of treatments for ALS, which has no effective therapy.
“This study will significantly advance the ALS field by providing a leading compound and a signaling pathway for future investigations,” said study leader Chun-Li Zhang, Ph.D., Professor of Molecular Biology and a W.W. Caruth, Jr. Scholar in Biomedical Research at UT Southwestern. Dr. Zhang is also an Investigator at the Peter O’Donnell Jr. Brain Institute at UTSW.
ALS, also known as Lou Gehrig’s disease, affects hundreds of thousands worldwide. With onset in midlife, ALS kills motor neurons over time, gradually depriving patients of the ability to walk, talk, swallow, and breathe. Life expectancy is two to five years after diagnosis and hasn’t changed despite decades of research, Dr. Zhang explained.
Searching for potential therapies that might extend the lives of ALS patients, Dr. Zhang and his colleagues tested compounds from a pharmaceutical library on a cellular model of ALS. Because it is impossible to sample motor neurons directly from ALS patients, previous studies have largely used neurons that were derived from pluripotent stem cells. However, Dr. Zhang said, these neurons were reset to an embryonic stage, losing age-related changes.
For the new study, the researchers used a different approach that converted ALS patients’ skin cells into motor neurons that bore marks of aging, providing a more realistic model. After dosing these cells with about 2,000 compounds, the researchers identified a promising one they dubbed Hit3.
This compound reversed some of the cells’ ALS-related morphological changes, causing them to grow larger cell bodies, develop more complicated branching in their extensions, form more connections with muscle cells, and live significantly longer than cells that didn’t receive Hit3.
A closer look showed that Hit3 acts on cell proteins called MAP4Ks, which play key roles in cells’ responses to stress. Once activated, MAP4Ks regulate a cascade of other proteins involved in this role, a molecular pathway that appears critical in deciding whether motor neurons live or die and has been implicated in ALS and other neurodegenerative diseases.
To determine what effect manipulating this pathway could have on ALS animal models, the researchers dosed mice that had mutations in a gene called SOD1—considered the most aggressive form of ALS—with a compound related to Hit3 called MAP4Ki. Mice that didn’t receive this compound had a dramatic loss of motor neurons and died at an average of 129 days. However, mice that received MAP4Ki maintained significantly more motor neurons and lived ten days longer.
“Even though MAP4Ki extended survival by just a short time, our results suggest treatments that block the MAP4K pathway could one day be useful therapeutically,” Dr. Zhang said.
Because MAP4Ki isn’t optimized for pharmaceutical use—it degrades quickly and can’t cross the blood-brain barrier, limiting its absorption—this compound has significant room for chemical manipulations that could improve its activity, Dr. Zhang said. In addition, he noted, because targeting the MAP4K pathway has shown promise, researchers could eventually develop other drugs designed to affect this pathway more successfully. The hope is that this could potentially extend ALS patients’ life span.
More information: Meng-Lu Liu et al, Screens in aging-relevant human ALS-motor neurons identify MAP4Ks as therapeutic targets for the disease, Cell Death & Disease (2024). DOI: 10.1038/s41419-023-06395-7
Provided by UT Southwestern Medical Center

Leave a Reply