JULY 3, 2024
by Rachel Martin, Yale University
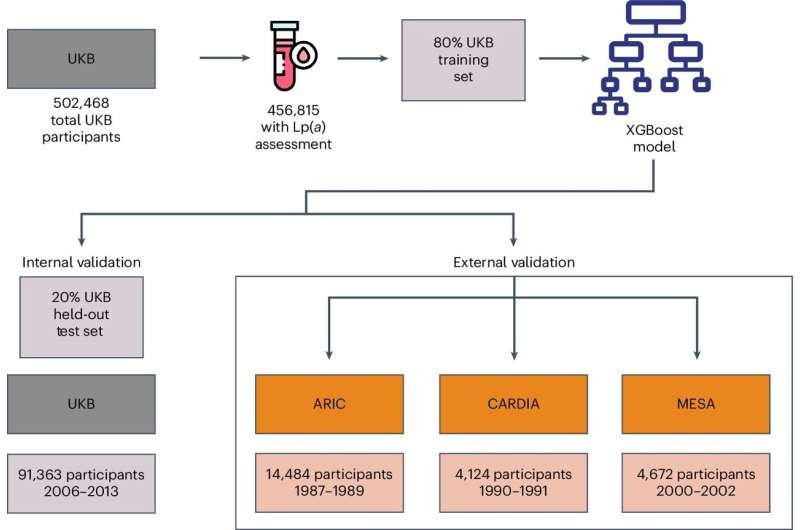
Study design. We developed and validated a machine learning model using structured clinical elements to optimize screening for elevated Lp(a), which can be deployed in clinical settings for case identification. Credit: Nature Cardiovascular Research (2024). DOI: 10.1038/s44161-024-00469-1
Many patients receive a standardized lipid panel as part of a yearly physical that includes testing of their “good” cholesterol (high-density lipoprotein) and “bad” cholesterol (low-density lipoprotein). However, most people are unfamiliar with another type of cholesterol, lipoprotein(a) or Lp(a). This type of lipoprotein is not included in the standard lipid panel but is an independent risk factor for cardiovascular disease.
In the following Q&A, Yale clinicians and researchers share background about Lp(a), guidance for caring for patients with elevated levels, and new approaches to improve testing.
What is lipoprotein(a)?
Lp(a)—which is pronounced as ‘lp little a’—is a lipoprotein whose serum level is genetically determined without much fluctuation after early childhood.
“We’ve known for many years that it is an independent risk factor for cardiovascular disease,” said Erica Spatz, MD, MHS, associate professor (cardiovascular medicine) and associate professor of epidemiology (chronic diseases).
“It contributes to atherosclerosis (plaque buildup in the heart arteries), thrombosis (blood clotting), and early aortic stenosis (narrowing of the valve that connects the main chamber of the heart to the rest of the body). It can also lead to major adverse cardiovascular events, like heart attacks.”
How is Lp(a) tested?
“It is checked with a simple blood test that is often covered by insurance,” said Spatz. “However, today, only about 0.5% of people in the United States are tested for Lp(a). This is because we haven’t had therapies to reduce Lp(a). It is not lowered by lifestyle interventions and statins, which are first-line agents for high cholesterol. So, it hasn’t been on most physicians’ radar to check.”
How can providers care for patients with elevated Lp(a) levels?
Although no targeted therapies are available, providers with expertise in preventive cardiology can work with patients to reduce risk.
“In our practice, we double down on all the other risk factors considered modifiable, like lifestyle and other LDL cholesterol,” said Spatz, who directs the Yale Preventive Cardiovascular Health Program, which provides care for patients at higher risk of developing cardiovascular conditions.
“If a person has cardiovascular disease and elevated Lp(a) levels, we may use non-statin medications, like PCSK9 inhibitors, because clinical trials showed greater benefit for these patients. We also recommend family members get tested.”
What research is in progress to help us better understand Lp(a)?
“We are excited about research in the pipeline that may give us new knowledge about how to treat patients with elevated Lp(a),” said Spatz. “I hope we will soon have some targeted treatment options. But the field of medicine needs to be prepared for a potential change in caring for these patients,” said Spatz.
“Unfortunately, enrollment in these clinical trials is slow,” added Rohan Khera, MD, MS, assistant professor of medicine (cardiovascular medicine), assistant professor of biostatistics (health informatics), and director of the Cardiovascular Data Science (CarDS) Lab.
“Only 1 in 8 people have elevated levels, so researchers need to test many people just to identify one who may be eligible for enrollment in the trial. To speed up research, we need a more efficient way to determine who would most benefit from testing.”
To meet this goal, the researchers recently conducted a study published in Nature Cardiovascular Research to find an approach to determine who would benefit most from testing. This is part of the strategy to create algorithmic diagnostics to improve health promotion at the population level.
How was the new screening tool developed?
The team of researchers developed a machine learning model that uses structured clinical elements found in the electronic health records to determine patients who most likely have elevated Lp(a) levels.
“While Lp(a) is an independent risk factor for cardiovascular disease, it does have company that it tends to keep,” Khera explained. “For example, we found that people with high Lp(a) were more likely to be women, Black, and to have hypertension or premature heart disease (presenting before the age of 60). They were also more likely to have a family history of atherosclerotic cardiovascular disease (ASCVD).”
The algorithmic model is based on the analysis of large, representative data sets, including the UK Biobank, ARIC, CARDIA, and MESA studies.
“We also evaluated the model to ensure that it was not introducing any bias in terms of social determinants of health, age, sex, race or ethnicity,” said Arya Aminorroaya, MD, MPH, postdoctoral associate in the CarDS Lab, and first author of the paper.
“The good news is that the model’s performance is consistent across all clinical subgroups. This tool is not going to replace the universal screening. But in this rapidly evolving landscape, this tool can help accelerate trial progress and help determine which patients will most benefit from screening.”
How can the new screening tool be used?
“This tool is not diagnostic. You still need to test the person,” said Khera. “But we have found that we can conduct half the number of tests to get the same number of patients with elevated levels.”
Khera, Spatz, Aminorroaya, and the team hope this tool will help researchers leading clinical trials determine how to select trial participants and help hospitals or health systems decide which patients may benefit most from screening.
“I also see the potential to take this tool directly to patients,” said Spatz. “Patients are aware of Lp(a) and wonder if they are at risk. This tool allows us to reach patients directly to help gauge their risk and prioritize testing in those at higher risk of elevated Lp(a).”
“This tool is not going to replace the universal screening, which is recommended by the European guideline and the National Lipid Association, and will likely be adopted more broadly soon,” said Aminorroaya. “But in this rapidly evolving landscape, this tool can help accelerate trial progress and help determine which patients will most benefit from screening.”
More information: Arya Aminorroaya et al, Development and multinational validation of an algorithmic strategy for high Lp(a) screening, Nature Cardiovascular Research (2024). DOI: 10.1038/s44161-024-00469-1
Journal information: Nature Cardiovascular Research

Leave a Reply