JULY 23, 2024
by UT Southwestern Medical Center
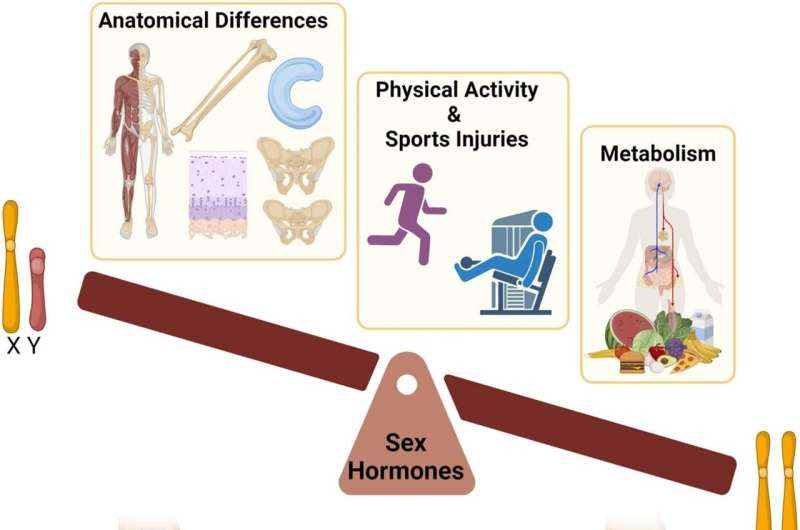
Contribution of biological sex (XX vs XY) and sex hormones to the development of OA. Credit: Osteoarthritis and Cartilage (2024). DOI: 10.1016/j.joca.2024.04.015
Sex-specific differences in the knee joint should be considered as early as childhood to help prevent higher incidence and severity of knee osteoarthritis (OA) in women later in life, UT Southwestern Medical Center researchers propose in a review of clinical data.
Their findings, published in Osteoarthritis and Cartilage, investigate knee anatomy and biology, metabolic factors, and youth sports injuries that can contribute to a higher risk of OA.
Osteoarthritis is the most common form of arthritis, with an estimated 33 million Americans living with the degenerative disease, according to the Centers for Disease Control and Prevention. Knee and hand joints have the highest prevalence of OA worldwide.
Although decades of research have established sex-specific variation in OA, the biological drivers of higher knee OA risk in females are not fully understood. As the frequency of knee injuries early in life increases OA risk, the need to identify prevention strategies becomes greater—particularly for women.
“The frequency and severity of sports-related injuries are on the rise, as it’s more common to see youths engaged in specialized sports with high demand at an early age,” said lead author Paula Hernandez, Ph.D., Instructor of Orthopedic Surgery and Biomedical Engineering at UT Southwestern.
“Young female athletes have a higher risk of ACL (anterior cruciate ligament) injuries compared to young male athletes, and we know these types of injuries can likely develop into OA later in life.”
By reviewing clinical data from multiple tissues within the knee joint, UTSW researchers revealed key factors behind sex differences from three perspectives: human anatomy, physical activity and response to injury, and metabolic signatures.
Data included mostly young but also older populations grouped into the categories of childhood (0–11 years), adolescence (12–18), early adulthood (19–49, premenopause), and late adulthood (50 and older, postmenopause) to compare across developmental stages.
Researchers found that differences between males and females in articular cartilage, meniscus, and ACL arise before puberty and can’t be explained solely by sex hormones. Although sex hormones such as estrogen and testosterone play a significant role, studies suggest sex chromosomes are also a driving factor.
Understanding the distinct roles of hormones and chromosomes may help clinicians regulate hormonal effects on OA risk.
The review also revealed intriguing variation between males and females in the abundance of amino acids and other metabolites, suggesting differences at the metabolic level.
The anatomic and metabolic distinctions between males and females revealed by the review—as well as social components in which gender affects lifestyle—play key roles in the likelihood of physical activity and injury early in life. In the case of knee OA, these differences increase risk for women.
Findings from this review and related research from Dr. Hernandez’s lab are expanding the field’s understanding of how OA is influenced by biological sex, laying groundwork that can be used for developing sex-specific exercises and wellness curriculum for students.
“We hope that by showing evidence that sex disparities are not limited to menopausal age, but rather commence early in life, we can create awareness for other researchers to start this practice,” Dr. Hernandez said.
More information: Paula A. Hernandez et al, Unraveling sex-specific risks of knee osteoarthritis before menopause: Do sex differences start early in life? Osteoarthritis and Cartilage (2024). DOI: 10.1016/j.joca.2024.04.015
Provided by UT Southwestern Medical Center

Leave a Reply