By Paul McClure
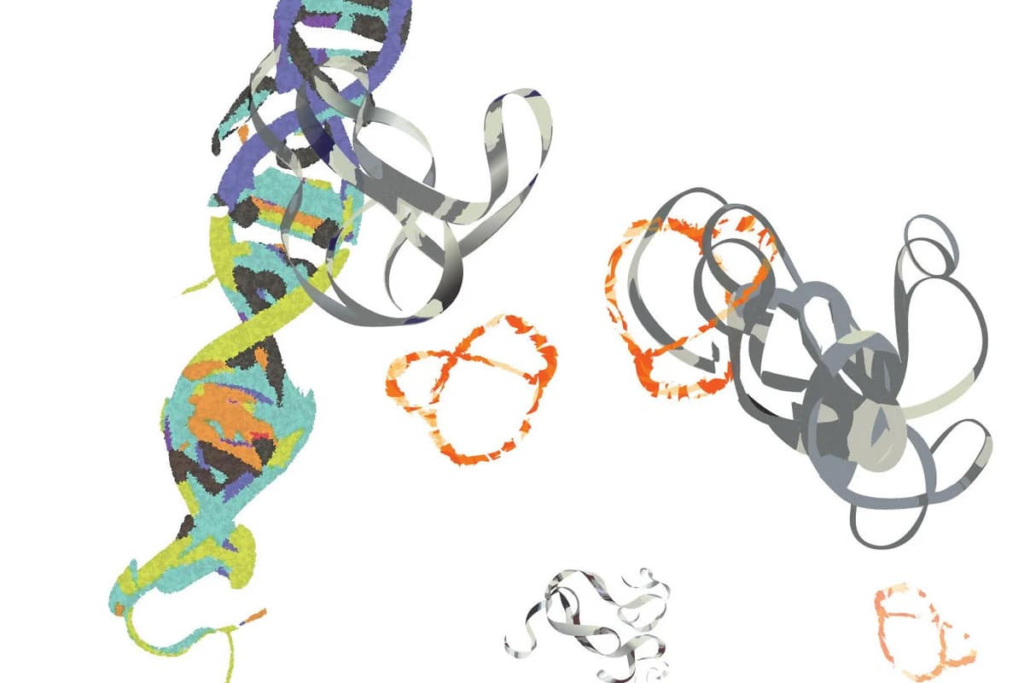
Researchers have developed a peptide (orange) that targets the MYC protein (gray ribbons) to slow cancer progressionMin Xue/UC Riverside
Researchers have developed a peptide that targets a previously ‘undruggable’ protein implicated in more than 75% of human cancers and found that it slowed the proliferation of brain cancer cells in the lab. It’s the first step towards developing an effective treatment for a range of cancers.
In healthy cells, the MYC protein is critical to the transcription process, where genetic information is converted from DNA to RNA and, eventually, into proteins. But, in cancer cells, MYC becomes unregulated and hyperactive, facilitating cancer initiation, maintenance, and progression by boosting transcription activities.
Because it’s implicated in more than 75% of all human cancer cases, MYC has long been one of the most attractive oncology drug targets. The problem is that MYC is a shapeless blob with no discernible binding pockets and a half-life of less than 30 minutes. So, despite decades of research, it’s remained ‘undruggable’. That is until researchers from the University of California Riverside (UC Riverside) discovered a peptide compound that binds to MYC, suppressing its activity.
“MYC is less like food for cancer cells and more like a steroid that promotes cancer’s rapid growth,” said Min Xue, one of the study’s corresponding authors. “It’s basically a glob of randomness. Conventional drug discovery pipelines rely on well-defined structures, and this does not exist for MYC.”
In a 2018 study, the researchers found that altering the shape and rigidity of a bicyclic peptide – a class of polypeptides with two loops in its structure – improves its ability to interact with structureless protein targets like MYC. The benefit of using bicyclic peptides as a basis for developing new peptide drugs is that they have the potential to bind to challenging drug targets with antibody-like submicromolar affinity and selectivity. In other words, they form a very strong, specific interaction with their target.
“Peptides can assume a variety of forms, shapes, and positions,” Xue said. “Once you bend and connect them to form rings, they cannot adopt other possible forms, so they then have a low level of randomness. This helps with the binding.”
The researchers built upon their previous work with bicyclic peptides, creating a library of second-generation peptides with better properties.
“We improved the binding performance of this peptide over previous versions by two orders of magnitude,” said Xue. “This makes it closer to our drug development goals.”
They screened the peptides in their library, identifying one – NT-B2R – that showed the highest binding affinity with MYC. To ensure that NT-B2R could bind to MYC in complex biological environments, the researchers tested it on a human glioblastoma cell line with known dependence on MYC activities. NT-B2R significantly affected the thermal properties of MYC, supporting direct interactions between them in a more complex binding environment.
The researchers then tested NT-B2R’s effect on cancer cells. Because the peptide is not cell-permeable, they used nanosized liposomes as delivery vehicles. The researchers observed that once NT-B2R was inside the cell, it bound to MYC, changing its physical properties and preventing it from performing transcriptional activities. NT-B2R treatment did not alter the expression and phosphorylation levels of MYC but did cause decreased metabolic activity and proliferation in human glioblastoma cells. RNA sequencing showed the treatment downregulated 704 genes and upregulated 1,322, consistent with MYC’s master transcription role. Genetic set enrichment analysis (GSEA) confirmed that MYC target gene sets were enriched, supporting that MYC was NT-B2R’s main target.
The disadvantages of using liposomes for drug delivery include high production costs and the potential for leakage of encapsulated drug molecules. For this reason, the researchers are developing an alternative that will effectively deliver NT-B2R into the cells. Future iterations of the peptide could lead to more potent MYC inhibitors.
“MYC represents chaos, basically, because it lacks structure,” Xue said. “That, and its direct impact on so many types of cancer, make it one of the holy grails of cancer drug development. We are very excited that it is now within our grasp.”
The study was published in the Journal of the American Chemical Society.
Source: UC Riverside

Leave a Reply