16 May 2024
By Gillian Dohrn
Scientists know there is a link between obesity and some cancers. A study in mice and people suggests why that might be.
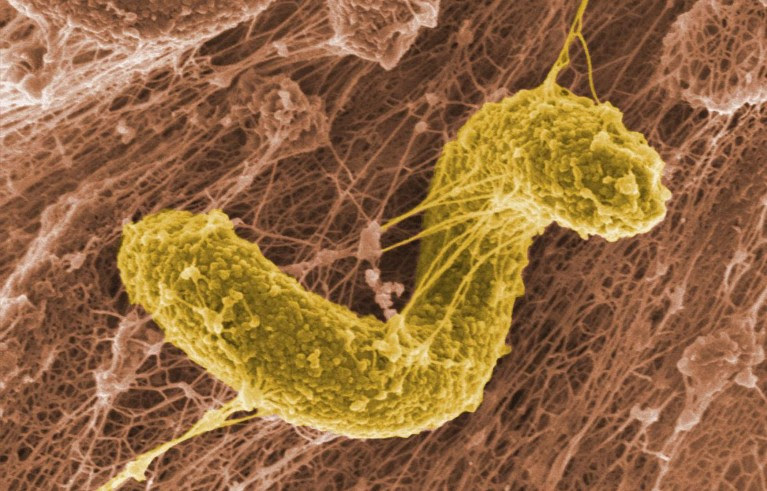
A Desulfovibrio bacterium. This group of gut bacteria has been linked to a suppressed immune system, which can allow breast-cancer tumours to flourish. Credit: PNWL/Alamy
Researchers have found a link between diet, a type of gut bacterium and breast cancer. The study, published on 6 May in the Proceedings of the National Academy of Science1, found that a high-fat diet increased the number of Desulfovibriobacteria in the guts of mice, suppressing their immune systems and accelerating tumour growth.
Researchers say the finding could spark new ideas for therapies for breast cancer, the most common malignancy affecting women worldwide.
Erwei Song, a breast-cancer surgeon at the SunYat-Sen Memorial Hospital in Guangzhou, China, and colleagues investigated the gut bacteria of people with breast cancer after collecting data showing that those with a high body-mass index had reduced chances of survival.
“A high-fat diet might promote progression of tumours or induce recurrence of tumours,” notes Song.
The researchers took tissue and fecal samples from 61 people with breast cancer at the SunYat-Sen Memorial Hospital, before the participants started treatment.
Women whose BMI exceeded 24 — the authors’ cut-off for obesity — had higher levels of bacteria in the Desulfovibrio genus than did those whose BMI was lower than 24.
The researchers then turned to mice to further explore this link. Mice that are fed a high-fat diet often serve as a proxy for human obesity in animal studies. The team found that mice consuming a high-fat diet had more Desulfovibrio bacteria and had elevated levels of a type of cell that suppresses the immune system, myeloid-derived suppressor cells (MDSCs), which originate in the bone marrow. This suggested to the researchers that higher numbers of Desulfovibrio bacteria and a suppressed immune system were linked; they just needed to find out how.
High-fat-diet mice also had higher levels of the amino acid leucine circulating in their blood than did mice fed a normal diet. Knowing that leucine can be made by some kinds of gut bacteria, the team treated the mice with antibiotics that killed Desulfovibrio. This caused both MDSC and leucine levels to return to normal.
Of mice and people
Armed with this information, the researchers went back to the blood samples that they had taken from the people with breast cancer. As anticipated, those with a BMI of more than 24 had higher levels of leucine, more immunosuppressive MDSCs and survived fewer years post-treatment than those with a lower BMI.
In other words, Desulfovibrio bacteria, benefiting from a high-fat diet, made excess leucine. This caused a spike in the numbers of MDSCs, which suppress the immune system and allow tumours to grow.
“It’s a provocative finding that will open up new avenues that we should be thinking about,” says Stephen Hursting, a nutritional biologist at the University of North Carolina at Chapel Hill.
Katherine Loree Cook, a cancer biologist focused on microbiome research at Wake Forest University School of Medicine in Winston-Salem, North Carolina, agrees, saying the study provides “strong evidence” of a new signalling mechanism involving gut bacteria.
“The influence of the microbiome on cancer development, disease progression and response to therapy is currently a critical area of research,” says Cook.

How gut microbes are joining the fight against cancer
But, she says, the composition of the gut microbiome can vary with geography and diet, so the findings might not translate to other populations. “Gut-microbiome studies across the world often report different populations associated with different outcomes,” she says.
But both Cook and Hursting see how the findings could lead to new treatment options. “If bacterial-derived leucine seems to be driving some of the cancer risk of a high-fat diet, how do we maybe reduce that, and encourage non-leucine-producing bacteria?” asks Hursting.
Hursting has studied leucine in the context of cancer cachexia, a wasting syndrome seen in people with certain cancers that causes severe weight loss, but hadn’t considered that high levels of it could be produced by gut microbes.
“This opened up a whole new avenue to me,” Hursting says.
References
Chen, J. et al. Proc. Natl Acad. Sci. USA 121, e2306776121 (2024).

Leave a Reply