Christina Szalinski
Lung cancer is the deadliest cancer in the world, largely because so many patients are diagnosed late.
Screening more patients could help, yet screening rates remain critically low. In the United States, only about 6% of eligible people get screened , according to the American Lung Association. Contrast that with screening rates for breast, cervical, and colorectal cancer, which all top 70%.
But what if lung cancer detection was as simple as taking a puff on an inhaler and following up with a urine test?
Researchers at the Massachusetts Institute of Technology (MIT), Cambridge, Massachusetts, have developed nanosensors that target lung cancer proteins and can be delivered via inhaler or nebulizer, according to research published this month in Science Advances. If the sensors spot these proteins, they produce a signal in the urine that can be detected with a paper test strip.
“It’s a more complex version of a pregnancy test, but it’s very simple to use,” said Qian Zhong, PhD, an MIT researcher and co-lead author of the study.
Currently, the only recommended screening test for lung cancer is low-dose CT. But not everyone has easy access to screening facilities, said the other co-lead author Edward Tan, PhD, a former MIT postdoc and currently a scientist at the biotech company Prime Medicine, Cambridge, Massachusetts.
“Our focus is to provide an alternative for the early detection of lung cancer that does not rely on resource-intensive infrastructure,” said Tan. “Most developing countries don’t have such resources” — and residents in some parts of the United States don’t have easy access, either, he said.
How It Works
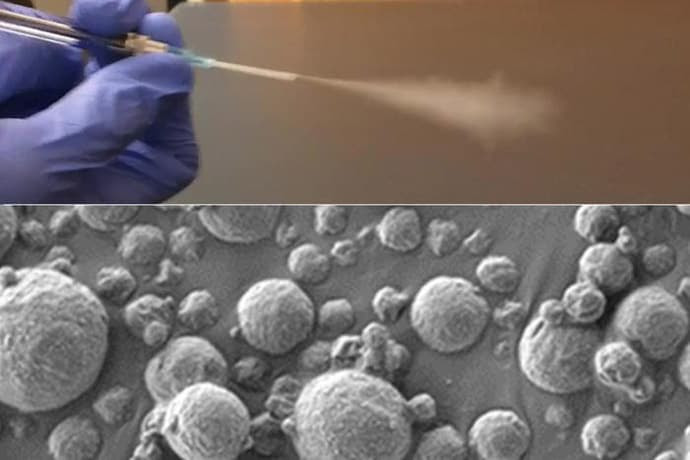
The sensors are polymer nanoparticles coated in DNA barcodes, short DNA sequences that are unique and easy to identify. The researchers engineered the particles to be targeted by protease enzymes linked to stage I lung adenocarcinoma. Upon contact, the proteases cleave off the barcodes, which make their way into the bloodstream and are excreted in urine. A test strip can detect them, revealing results about 20 minutes from the time it’s dipped.
photo of lung cancerNanosensors that target lung cancer proteins can be aerosolized and delivered with an inhaler or nebulizer.
The researchers tested this system in mice genetically engineered to develop human-like lung tumors. Using aerosol nebulizers, they delivered 20 sensors to mice with the equivalent of stage I or II cancer. Using a machine learning algorithm, they identified the four most accurate sensors. With 100% specificity, those four sensors exhibited sensitivity of 84.6%.
“One advantage of using inhalation is that it’s noninvasive, and another advantage is that it distributes across the lung quite homogeneously,” said Tan. The time from inhalation to detection is also relatively fast — in mice, the whole process took about 2 hours, and Zhong speculated that it would not be much longer in humans.
Other Applications and Challenges
An injectable version of this technology, also developed at MIT, has already been tested in a phase 1 clinical trial for diagnosing liver cancer and nonalcoholic steatohepatitis. The injection also works in tandem with a urine test, the researchers showed in 2021. According to Tan, his research group (led by Sangeeta Bhatia, MD, PhD) was the first to describe this type of technology to screen for diseases.
The lab is also working toward using inhalable sensors to distinguish between viral, bacterial, and fungal pneumonia. And the technology could also be used to diagnose other lung conditions like asthma and chronic obstructive pulmonary disease, Tan said.
The tech is certainly “innovative,” remarked Gaetano Rocco, MD, a thoracic surgeon and lung cancer researcher at Memorial Sloan Kettering Cancer Center, Middletown, New Jersey, who was not involved in the study.
Still, challenges may arise when applying it to people. Many factors are involved in regulating fluid volume, potentially interfering with the ability to detect the compounds in the urine, Rocco said. Diet, hydration, drug interference, renal function, and some chronic diseases could all limit effectiveness.
Another challenge: Human cancer can be more heterogeneous (containing different kinds of cancer cells), so four sensors may not be enough, Zhong said. He and colleagues are beginning to analyze human biopsy samples to see whether the same sensors that worked in mice would also work in humans. If all goes well, they hope to do studies on humans or nonhuman primates.

Leave a Reply