by The Francis Crick Institute
Support cells in the nervous system help protect motor neurons in the early-stages of sporadic motor neuron disease, according to new research from the Crick and UCL.
Motor neuron disease is a degenerative condition which destroys the nerve cells (motor neurons) in the brain and spinal cord, which control movement, speech, swallowing and breathing. The most common type of motor neuron disease is amyotrophic lateral sclerosis (ALS), which affects around 5,000 people in the UK at any one time.
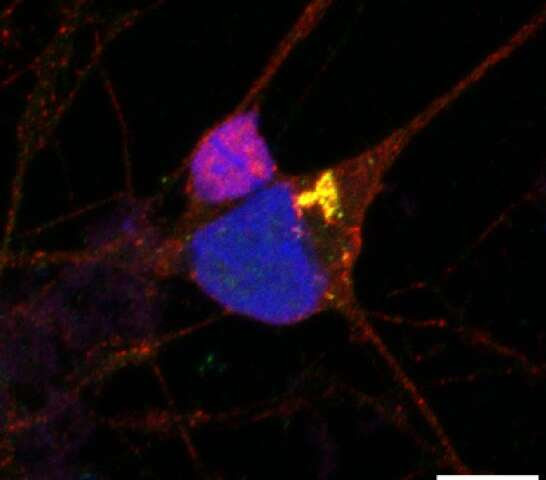
The study, published in Brain, found that in this disease, the motor neurons in the brain and spinal cord become sick and die when a protein, called TDP-43, misfolds and accumulates in the wrong place within the motor neurons. Conversely, when this happens in a type of cell that supports motor neurons, called astrocytes, these cellsappear comparatively resistant and survive.
When these two types of cells are close together, the more-resistant astrocytes are able to protect motor neurons from the misfolded protein. This rescue-mechanism helps the motor neurons, which are needed to control muscles, live longer.
“The role astrocytes have played in dealing with toxic forms of TDP-43 in motor neurons has not been previously well documented in motor neuron disease. It’s exciting that we’ve now found that they may play an important protective role in the early-stages of this disease,” explains Phillip Smethurst, lead author and former postdoc in the Human Stem Cells and Neurodegeneration Laboratory at the Crick. “This has huge therapeutic potential—finding ways to harness the protective properties of astrocytes could pave the way to new treatments. This could prolong their rescue function or find a way to mimic their behaviour in motor neurons so that they can protect themselves from the toxic protein.”
This research also established a new model for studying motor neuron disease. This new method more closely resembles the disease in patients as it uses healthy human stem cells, derived from skin cells, and spinal cord tissue samples donated by patients with motor neuron disease, collected post-mortem.
“It is thanks to the selfless donations from people with motor neuron disease, that we were able to study the interplay between motor neurons and astrocytes in conditions that closely resemble what happens in humans. These human cell models are a powerful tool for further studies of motor neuron disease and in the hunt for effective therapies,” explains Katie Sidle, co-senior author, neuroscientist and consultant neurologist at the National Hospital for Neurology in Queen Square, University College London Hospitals.
“For the first time, we have been able to create a model of sporadic motor neuron disease by essentially ‘transferring’ the toxic TDP-43 protein from post-mortem tissue into healthy human stem cell-derived motor neurons and astrocytes in order to understand how each cell type responds to this insult, both in isolation and when mixed together. The insights made in this work are testament to the power of creative collaboration and interdisciplinarity. It is through many years working together as a group of clinicians, pathologists, stem cell biologists, protein biochemists and other experts, and with a joint aim of increasing knowledge about motor neuron disease (to ultimately help find a cure), that these results have been possible,” says Rickie Patani, co-senior author, group leader of the Human Stem Cells and Neurodegeneration Laboratory at the Crick, consultant neurologist at the National Hospital for Neurology in Queen Square, University College London Hospitals and Professor of Human Stem Cells and Regenerative Neurology at UCL Queen Square Institute of Neurology.

Leave a Reply