by Ben Knight, University of New South Wales
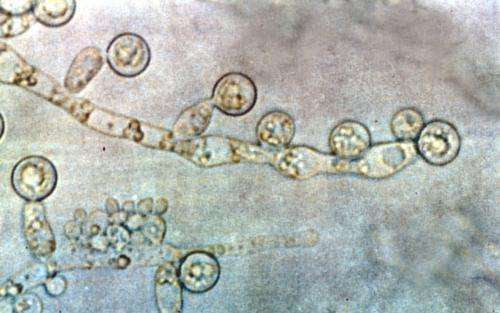
Candida albicans. Credit: Wikipedia.
Thinking of fungi probably conjures up an image of some wild mushrooms or a sourdough starter in your mind. That, or maybe a time where you had an unfortunate itchy skin rash that went away with a bit of topical medication.
But researchers in mycology—the study of fungi—have long warned that fungi can have a much more sinister side. While we’re unlikely to see a pandemic play out—certainly not along the lines of scenarios portrayed in fictional TV series “The Last of Us”—real-life scientists are worried about rising rates and severity of fungal infections worldwide.
“Fungi have historically been overlooked in infectious disease research,” says Dr. Megan Lenardon, a microbiologist and a senior lecturer in UNSW’s School of Biotechnology and Biomolecular Sciences. “There are many pathogens with different transmission routes and many challenges with therapies and diagnostics.”
An emerging fungal threat
The threat of fungal pathogens is now gaining worldwide attention from public health bodies. The World Health Organization recently released its first-ever watchlist of fungal priority pathogens—species of highest concern that require serious attention.
Dr. Lenardon has been studying the cell and molecular biology of Candida albicans, which was identified as one of the four fungi of critical priority. Candida species cause non-serious infections like thrush in tens of millions of people per year. But of more concern are the 700,000 invasive infections that can kill people, about half of which are caused by C. albicans.
“We call them ‘opportunistic invasive’ fungal pathogens because they don’t kill healthy people,” Dr. Lenardon says. “But if they find themselves in a host who is susceptible, then they can kill.”
Some fungi, like Aspergillus and Cryptococcus, are breathed in through spores that exist everywhere in the environment but are usually no match for our immune systems. Others, like C. albicans, colonize the gut of healthy individuals, but the physical barrier between the bloodstream, gut microbiota and a firing immune system is generally enough to prevent infections.
But when these defenses are compromised, it can leave us vulnerable to infection. In immunocompromised people, C. albicans can escape the gut, circulate throughout the blood, and invade organs.
“Serious fungal infections are more of a risk for people with underlying health conditions,” Dr. Lenardon says. “People with cancer or HIV/AIDS, organ transplant recipients, and intensive care patients are among those who are more vulnerable to infection.”
While the likelihood of acquiring a severe fungal infection is rare, infection is often deadly. At least 40% of systemic C. albicans infections are fatal despite the availability of antifungals. By comparison, a nasty bacterial infection like Staphylococcus aureus (golden staph) kills in around 25% of cases.
According to new estimates, there are 6.5 million invasive infections and 3.8 million deaths globally each year associated with severe fungal disease.
“The number of deaths from fungal infections is also likely underreported,” Dr. Lenardon says. “Usually, an existing health condition is recorded as the cause of death when the fungal infection was responsible.”
Provided by University of New South Wales

Leave a Reply