July 29, 2024
by Fujita Health University
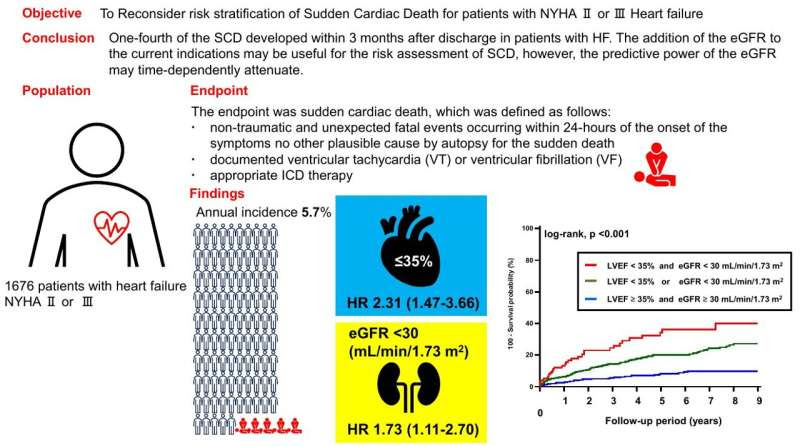
This study by Fujita Health University researchers revealed that kidney function, considered in terms of estimated glomerular filtration rate (eGFR), can be used as a predictor for SCD in patients with congestive heart failure. Credit: Yoshihiro Sobue from Fujita Health University
Patients with congestive heart failure (CHF) having a compromised blood supply, are at greater risk of sudden cardiac death (SCD). With an estimated incidence as high as 22% among these patients, current clinical guidelines recommend using implantable cardioverter defibrillators (ICDs) to help mitigate the risk of SCD.
Although the application of ICDs in patients with CHF is backed by substantial evidence, these studies did not include people with chronic kidney disease (CKD), who are an important clinical population. In other words, it is unclear whether the use of ICDs is justified in patients with CKD, especially with mild and moderate presentations, given the inherent risk involved in installing these devices.
To address this knowledge gap, researchers led by Associate Professor Yoshihiro Sobue from Fujita Health University, Japan, investigated to what extent kidney function can be a good predictor for the risk of SCD. This study was published in ESC Heart Failure on June 10 2024, and was co-authored by Hideo Izawa, also from Fujita Health University, and Eiichi Watanabe from Fujita Health University Bantane Hospital.
Elaborating on the rationale behind this examination, Dr. Sobue says, “The objective of our study was to prospectively investigate the risk factors for SCD in a cohort of over 1,500 patients hospitalized with CHF classified based on the left ventricular ejection fraction (LVEF) and the New York Heart Association (NYHA) functional class, as well as the potential role of kidney function as a determinant of SCD.”
Adding further to the importance of using renal dysfunction for SCD, he says, “The determination of renal dysfunction as an independent risk factor of SCD is important because patients with moderate-to-severe renal dysfunction were excluded in the studies on which current ICD implantation guidelines are based.”
The study ultimately included 1,676 patients who had visited Fujita Health University Hospital for decompensated heart failure. During the follow-up period, 198 of these patients suffered from SCD. Among these events, 23% occurred within 3 months of discharge.
In conducting statistical analyses of the gathered data, the research team identified two key independent predictors for the risk of SCD following discharge. The first was LVEF, which is already considered in the current guidelines. The second was the estimated glomerular filtration rate (eGFR), which is a measure of how well the kidneys can filter blood.
By adding eGFR as a predictor alongside LVEF, regression models could predict SCD more accurately. However, as the researchers noted, the predictive power of kidney function in this way diminished over time, being more effective in the first few months after discharge. Coincidentally, roughly a quarter of all cases of SCD occurred within three months of discharge.
In summary, the findings of this study underline the importance of considering additional factors, such as kidney condition, when weighing the benefits of using ICD in a patient.
“Refining the criteria for ICD implantation holds the potential for significantly improving the prevention of SCD and reducing the incidence of complications arising from unnecessary ICD implantations. Hopefully, applying an enhanced stratification methodology involving eGFR may yield better clinical outcomes,” remarks Dr. Sobue.
In the long term, these findings may steer the way for the revision of guidelines for the use of ICDs and improve the outcomes for patients with CHF, both with and without CKD.
More information: Yoshihiro Sobue et al, Renal dysfunction is a time‐varying risk predictor of sudden cardiac death in heart failure, ESC Heart Failure (2024). DOI: 10.1002/ehf2.14892
Provided by Fujita Health University

Leave a Reply