by Elodie Smith, Cornell University
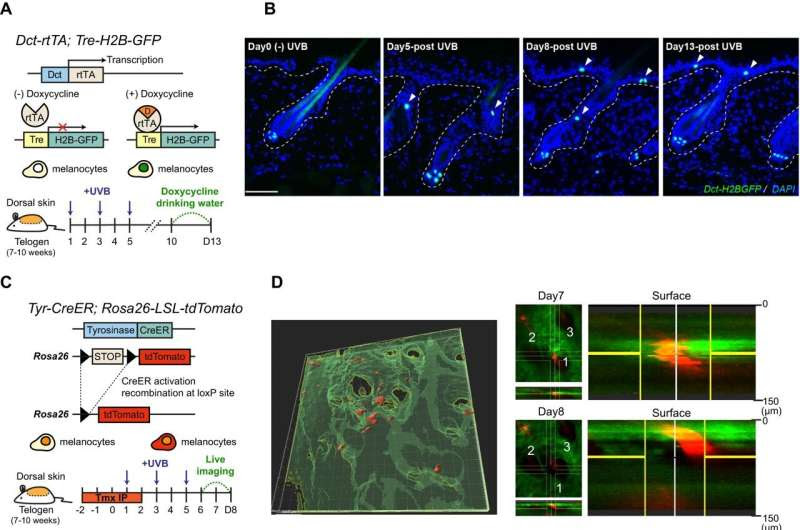
Tracking recruitment of hair follicle McSCs to the epidermis by UVB on unpigmented mouse dorsal skin. Credit: Nature Communications (2024). DOI: 10.1038/s41467-024-45034-3
Patients with an appearance-altering skin condition may have relief thanks to an unlikely cocktail of a molecule that induces labor, an immunosuppressant medication and controlled UVB irradiation.
This College of Veterinary Medicine-led discovery, published in Nature Communications, uses drugs already approved by the FDA, speeding the path of a brand-new treatment for the disease, vitiligo, to clinical trials.
Vitiligo occurs when the immune system destroys skin melanocytes—the cells that create melanin to give color and protection to the skin. As a result, patients’ skin has white de-pigmented patches, which can cause social stigma and a decreased quality of life.
Most existing drugs treat the autoimmune aspect of vitiligo, stopping the destruction of melanocytes. However, these medications rarely lead to a full and long-lasting pigmentation of the skin.
“We wanted to find ways to re-pigment the skin in a more durable and more complete way,” said Andrew White, associate professor in the Department of Biomedical Sciences, and lead author of the study. To do that, White took an approach based on controlled UVB irradiation.
White’s idea was inspired by a 2013 scientific paper detailing how UVB triggers the movement of melanocytes from hair follicles to the skin. However, why exactly UVB caused the migration, and how to control the process, was unknown.
“There was basically no protocol for what we were trying to do,” White said.
Luye An, a doctoral student in White’s lab, led the study.
Using mouse models to study the disease, the team exposed the white skin of black-coated mice to UVB, and induced the melanocytes in the mice’s follicles to migrate toward their skin, just like the 2013 study.
However, in this case, the experiments revealed something puzzling: The response differed between males and females. Initially unaware of the sex differences, the researchers sometimes observed a lot of melanocyte migration and sometimes very little, depending on the mice they randomly selected.
“Initially, it was frustrating and confusing,” White said. “The sexual dimorphism was unexpected, but when we figured it out, it was really exciting.”
The team discovered that UVB exposure triggers an inflammatory response in the skin, which is much higher in males than in females, who show lower inflammation and little melanocyte migration. Analyzing the gene expression between males and females revealed that the males’ higher skin inflammation in response to UVB was due to a higher production of prostaglandins, a group of molecules that are produced in response to injury and tissue damage. Literature searches showed that prostaglandins could stimulate melanocytes in various ways.
To confirm the effect of prostaglandin, the researchers exposed the mice’s white skin to UVB before injecting it with a prostaglandin solution. They observed that, with prostaglandin, the melanocyte migration from hair to skin was higher than with UVB alone, and became as high in females as in males.
More information: Luye An et al, Sexual dimorphism in melanocyte stem cell behavior reveals combinational therapeutic strategies for cutaneous repigmentation, Nature Communications (2024). DOI: 10.1038/s41467-024-45034-3
Provided by Cornell University

Leave a Reply