by NIH/National Heart, Lung and Blood Institute
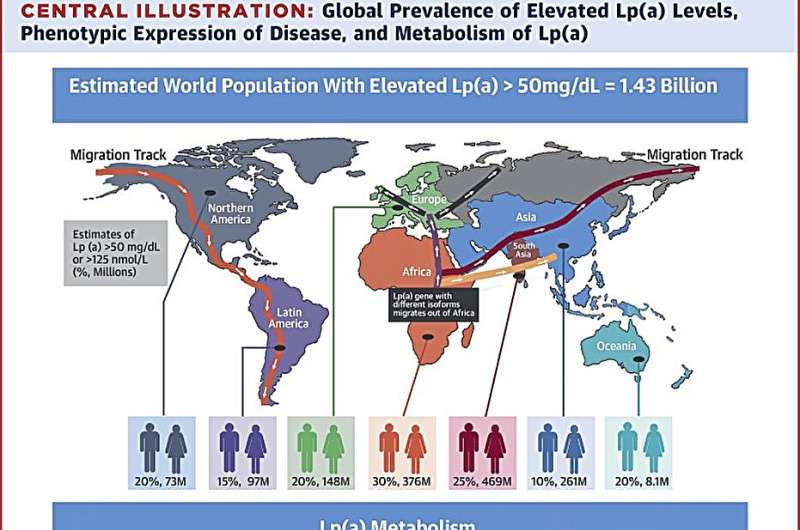
Central Illustration. Credit: Journal of the American College of Cardiology (2018). DOI: 10.1016/j.jacc.2017.11.014
If you’ve listened to the radio or opened a webpage in the past year, you may have seen or heard ads promoting lipoprotein(a), or Lp(a), testing to help people identify risks for heart disease.
But, what is Lp(a)? Most importantly: should you get your levels tested?
Lp(a) is a type of lipid, or fat, in the body that contains and is similar in structure to low-density lipoprotein (LDL) cholesterol, often thought of as “bad cholesterol.” Like LDL cholesterol, Lp(a) deposits cholesterol in the arteries and can show up in plaque. It’s also found in cells that line small blood vessels and in tissues where regeneration and healing occur.
“There is a lot of intrigue about it,” said Sotirios Tsimikas, M.D., an Lp(a) researcher and professor of medicine at the University of California San Diego. “Is it just an error of evolution that became very common? Does it have a physiological function? We don’t know.”
The lipoprotein’s composition, which includes other lipoproteins, has also made it a prime research target. “Lp(a) is more complex than LDL,” said Lijuan Liu, Ph.D., a program officer specializing in lipid metabolism and atherosclerosis in the Division of Cardiovascular Sciences at NHLBI.
“It seems to have all the same bad features as LDL,” added Alan T. Remaley, M.D., Ph.D., a senior investigator in NHLBI’s Lipoprotein Metabolism Laboratory, “but some extra harmful features that we don’t fully understand.” For example, he explained that Lp(a) acts as a molecule that supports clotting, and this, among other features, appears to make it even worse than LDL as a risk marker for cardiovascular disease.
Here’s more of what researchers have found about Lp(a) and what studies may soon reveal:
Elevated Lp(a) levels are a cardiovascular disease risk factor
For decades increased Lp(a) levels have been linked to a higher risk for cardiovascular disease. This now includes heart attack, stroke, and a range of conditions like irregular heart rhythms, heart valve disease, and limited lower-body circulation.
The connections crystalized in the late 1990s when researchers, like those in Tsimikas’ lab, started seeing more patients with elevated Lp(a) levels who needed coronary revascularizations, a procedure to restore blood flow to and around the heart.
Around the same time, the researchers learned about how Lp(a) was linked to inflammation, which tracked with what they saw at the hospital. Genetic studies soon found that some people had different expressions of the LPA gene, which could increase their risk of having elevated Lp(a) levels.
Today, about 20-30% of people worldwide are estimated to have elevated Lp(a) levels, which are generally thought to start between 30-50 mg/dL.
Tsimikas explained that Lp(a) is likely the leading inherited risk for cardiovascular disease. “It’s more heritable than hypertension, diabetes, and obesity,” he said. However, “Even if the level is elevated, it doesn’t mean you will have an event. It just puts you at a higher risk.”
Preventive screenings are increasingly used to gauge risks
Reassuringly, most people—about 70-75%—would have low Lp(a) levels if they were screened today, said Tsimikas. Preventive screenings are designed to identify the smaller proportion of people with elevated levels.
In the U.S., Lp(a) testing is recommended for people younger than age 65 who have had a heart attack, those with a family history of premature heart disease, and those with elevated LDL cholesterol who haven’t responded to statins, cholesterol-lowering drugs that can lower LDL levels by about 30%.
Since elevated Lp(a) levels are largely due to genetic risks and don’t fluctuate much in response to modifiable risks, such as exercise, a one-time screening would be sufficient for most people, the experts noted. In Europe and Canada, Lp(a) screenings are recommended for everyone.
Large clinical trials are testing Lp(a)-lowering therapies
Currently, if a person has elevated Lp(a) levels, they would likely work with their physician to create a plan to take steps to support heart-healthy living and minimize any risks, such as having high blood pressure or high cholesterol.
Some patients may also consider taking LDL cholesterol-lowering treatments, such as statins or PCSK9 inhibitors. In some cases, PCSK9 inhibitors have been shown to lower Lp(a) levels by about 20-30%. Lipoprotein apheresis, which removes excess Lp(a) and LDL cholesterol from the body, is another option, but for people with higher risks.
Researchers are also studying targeted approaches to lower Lp(a) and approaches to support patients further. Tsimikas is studying aspirin’s effect in reducing inflammation in people with elevated Lp(a) levels. Additionally, other research, conducted through a large phase 3 trial is testing if a medication can lower Lp(a) levels.
Another trial is studying how to block its production. Results from both studies will be available in about two to three years.
A secondary focus of ongoing Lp(a) research is to identify if and when benefits occur at different points of intervention. Participants in the phase 3 studies have Lp(a) levels between 70-80 mg/dL. Future studies may find lowering Lp(a) to levels below 50 mg/dL or 20-30 mg/dL has benefits, but it’s too early to tell, said Tsimikas. “We’ll have to let the science drive us to decide at what Lp(a) level we should start thinking about treating Lp(a) as a risk factor,” he explained.
“We’re hopeful,” Tsimikas said about the research. This is why he often tells parents he meets who have a young child with elevated Lp(a) levels to stay optimistic. “I tell them that by the time your 7-year-old has to worry about this, we’ll have a way to treat it.”
Journal information: Journal of the American College of Cardiology
Provided by NIH/National Heart, Lung and Blood Institute

Leave a Reply