by American Heart Association
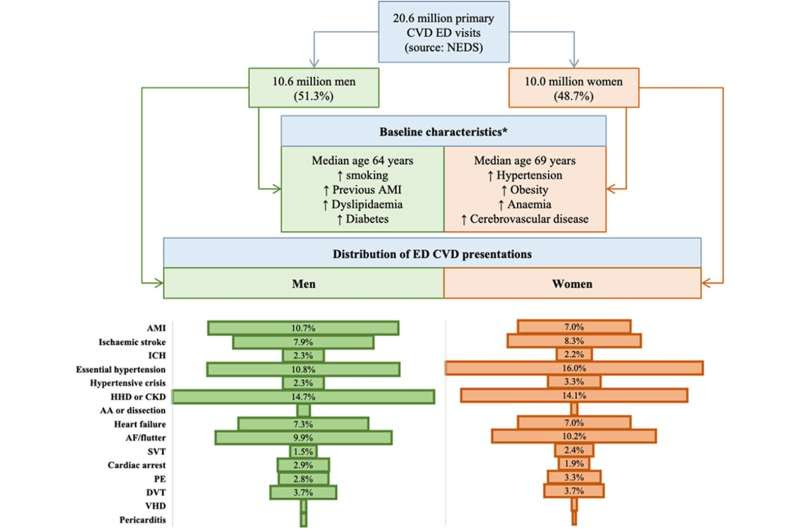
Overview of study sample and sex distribution of emergency department (ED) cardiovascular presentations. *Arrows indicate relative frequency of risk factor (eg, there were more smokers among men than women). AA indicates aortic aneurysm; AF, atrial fibrillation; AMI, acute myocardial infarction; CKD, chronic kidney disease (hypertensive); CVD, cardiovascular disease; DVT, deep vein thrombosis; HHD, hypertensive heart disease; ICH, intracranial hemorrhage; NEDS, Nationwide Emergency Department Sample; PE, pulmonary embolism; SVT, supraventricular tachycardia; and VHD, valvular heart disease. Credit: Journal of the American Heart Association (2022). DOI: 10.1161/JAHA.122.026432
The top cardiovascular (CVD) diagnoses from U.S. emergency departments suggest that many cardiovascular emergencies are due to poorly controlled high blood pressure, according to a study of more than 20 million emergency department visits published Sept. 8 in the Journal of the American Heart Association, an open access, peer-reviewed journal of the American Heart Association.
The researchers found that 13% of all heart-related emergency department diagnoses, representing more than 2.7 million people, were for “essential” hypertension, which is high blood pressure not caused by other diseases. Most cases of high blood pressure are essential hypertension.
“These visits resulted in hospital admission less than 3% of the time and with very few deaths—less than 0.1%. This suggests that these visits were mostly related to the management of hypertension,” said lead author Mamas A. Mamas, M.D., a professor of cardiology at Keele University in Stoke-on-Trent, and a consultant cardiologist at University Hospitals of North Midlands NHS Trust, both in the UK.
For the 15 CVD conditions detailed in the study, about 30% were hypertension-related diagnoses.
The study analyzed cardiovascular diagnoses made during emergency department visits that were part of the Nationwide Emergency Department Sample from 2016-2018. The sample was 48.7% women, and the average age was 67 years. The majority were Medicare or Medicaid participants. Men in the sample were more likely to have other diseases in addition to cardiovascular disease, such as diabetes, while women had higher rates of obesity, high blood pressure and medical conditions that affect blood vessels in the brain.
The most common heart- or stroke-related diagnoses for women seen in the emergency department were high blood pressure (16% of visits), high blood pressure-related heart or kidney disease (14.1%) and atrial fibrillation (10.2%). The most common diagnoses for men were high blood pressure-related heart or kidney disease (14.7%), high blood pressure (10.8%) and heart attack (10.7%).
“Previous studies have shown sex differences in patterns of CVD among hospitalized patients,” Mamas said. “However, examining CVD encounters in the emergency department provides a more complete picture of the cardiovascular health care needs of men and women, as it captures encounters prior to hospitalization.” He also points out that previous studies of CVD emergency visits are limited to suspected heart attack visits. “Therefore, this analysis of 15 CVD conditions helps to better understand the full spectrum of acute CVD needs, including sex disparities in hospitalization and risk of death.”
The study found that outcomes from the emergency CVD visits were slightly different for men and women. Overall, women were less likely to die (3.3% of women vs 4.3% of men) or be hospitalized (49.1% of women vs 52.3% of men) after an emergency department visit for CVD. The difference may be due to women’s generally lower risk diagnoses, said Mamas, but there could be an underestimation of deaths in women.
“We did not track deaths outside of the hospital setting,” said Mamas. “Given past evidence that women are more likely to be inappropriately discharged from the emergency department, and strong evidence for the systemic undertreatment of women, further study is warranted to track outcomes beyond the emergency department visit.”
An additional limitation of the data includes potential misdiagnosis errors in cases where the final diagnosis did not match the emergency diagnosis, particularly after a hospitalization and additional bloodwork and other health information could be obtained. Furthermore, the data is limited in that it does not capture information related to severity of disease, which may make comparisons around mortality differences between different patient groups challenging.
“Our work with this large, nationally representative sample of cardiovascular emergency visits highlights differences in health care needs of men and women, which may be useful to inform planning and provision of health care services,” said Mamas. “We also encourage further research into understanding the underlying factors driving the differences in CVD patterns and outcomes between men and women.”

Leave a Reply