Two men in China were the first people in the world to receive an experimental treatment for heart disease based on ‘reprogrammed’ stem cells and have recovered successfully one year later, says the cardiac surgeon who performed the procedures. In May last year, the men were injected with heart muscle cells derived from induced pluripotent stem (iPS) cells, the surgeon told Nature — the first known clinical application of iPS-cell technology for treating damaged hearts.
No results have yet been published, so researchers not involved in the work have cautioned that there is no way to confirm whether the treatment works, including whether the reported benefits are due to the iPS-derived cells or simply to the heart bypass that accompanied the treatment.
But the surgeon, Wang Dongjin at Nanjing Drum Tower Hospital, spoke to Nature in detail about the procedure and about the patients’ conditions. And one of the men, Han Dayong, a 55-year-old electrician from Yangzhou in eastern China who received the treatment alongside a heart bypass says he is very satisfied with the outcome. Before the surgery, Dayong remembers being tired and often out of breath. Now he can go for walks, climb stairs and sleep through the night. “It was beyond my expectations,” he says.
The team plan to publish the results from the two patients later this year, says Wang Jiaxian, who heads the Nanjing-based biotechnology company HELP Therapeutics that supplied the heart muscle cells, known as cardiomyocytes, used in the study. They also have approval to expand their study to include a further 20 patients, he says.
The trial in China, which is listed on a global clinical trial registry, is not the only one that is ongoing. In January a cardiac surgeon in Japan, Yoshiki Sawa, introduced iPS-derived cardiomyocytes designed to treat heart disease into a patient — which media reported at the time was a world first. The team are using an alternative approach in which sheets of cells are grafted onto the heart rather than injected into the organ.
Muscle morph
For decades, researchers have been trying to treat heart disease — a leading cause of death worldwide — using adult stem cells. They hoped that the cells would morph into muscle cells once inserted into the heart.
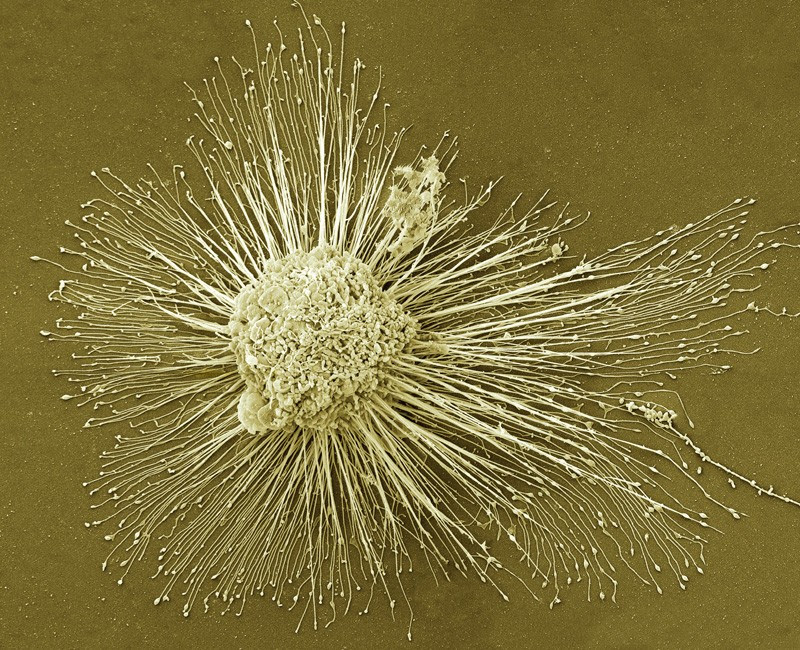
But after trials in people proved inconclusive, researchers turned to iPS cells. These are created by inducing adult cells to revert to an embryonic-like state, from which they can develop into other cell types, such as cardiomyocytes. Work with iPS cells is less ethically fraught than that using embryonic stem cells, which can also differentiate into many other cell types.
Evidence in rodents and monkeys suggests that introducing iPS-cell-derived cardiomyocytes directly into the heart does regenerate muscle tissue and improve the organ’s function1,2. Researchers hope that the first trials in people will reveal the same.
“These are really exciting times,” says Wolfram-Hubertus Zimmermann, a pharmacologist at the University Medical Centre Göttingen in Germany.
He says the first trial in people sounds promising, but because they have not been published there is no way to confirm whether the treatment works.
The potent effects of Japan’s stem-cell policies
As well as the iPS-cell pilot study underway in Japan, several others are planned in France and the United States. Zimmermann is also planning one in Germany.
But researchers are divided over how cardiomyocytes might repair the heart, and whether the best way to introduce them is by direct injection or a graft.
“We are going to see a lot of interesting shots on goal in the next five years. We don’t know what the answer is going to be. It is time to let the patients teach us,” says Charles Murry, a pathologist at the University of Washington in Seattle who also plans to inject cells into people’s hearts.
Safety first
That there is a trial ongoing in China came as a surprise to many, who didn’t know that researchers there had overcome one of the field’s biggest challenges — the ability to produce large numbers of iPS-cell-derived cardiomyocytes that are pure enough to be used in people. This takes a lot of time and effort to get right, so very few companies or research groups have successfully done it, says Murry.
Wang Jiaxian says that his company has been developing the cells for almost four years.
Wang Dongjin told Nature that he injected some 100 million cardiomyocytes, derived from iPS cells created using cells donated by a healthy person, around the damaged heart tissue of his two patients. At the same time, both men, who had severe heart disease, underwent a coronary artery bypass operation, in which vessels from elsewhere in the body are transplanted onto the artery to improve blood flow.
Wang says his goal was to assess the safety of the cell injections, and that he was encouraged when his patients’ heart function improved significantly after the operation. Neither patient has developed tumours, he adds, which can be a risk of using pluripotent stem cells.
To prevent the body from attacking the cardiomyocytes, Wang says that both patients took immunosuppressant drugs, one patient took them for a month and the other had to stop after a week owing to side effects. Both men were discharged from hospital less than a month after surgery, he says.
Wang also says that the procedure did not cause sustained dysfunction in cardiac rhythm. Zimmermann says that is a sign that it’s safe, although it needs to be trialled in more people to be sure. But the apparent safety of the treatment might also be explained by the low dose of cells the team reportedly used, he says.
Murry adds that the health benefits the patients have reported cannot be attributed to the reprogrammed cells alone, because the men also received a coronary bypass. “If you do two things to somebody and they get better, you can’t say which one caused it,” he says.
Best approach
Researchers are divided on the best approach to introduce cardiomyocytes into the heart. Injecting them is typically less intrusive than grafting sheets of cells, because it doesn’t require surgery, although the Chinese patients did have surgery for the bypass. Proponents of injections also argue that in animals, the procedure allowed the tissue to better integrate into the heart and produce new muscle3.
But Philippe Menasché, a cardiac surgeon at the University of Paris, says that the injections puncture the organ in multiple locations, which might damage the tissue. The approach is also not easily reproduced, because the cells are injected somewhat randomly, and sometimes cluster, which could contribute to irregular beating of the heart, he adds.
Wang says his patients experienced short bouts of irregular beating, but it was not sustained.

Japan approves first human-animal embryo experiments
In January, cardiac surgeon Yoshiki Sawa at Osaka University performed the first in-person trial of the alternative approach; grafting sheets of 100 million cardiac muscle cells — derived from a healthy donor — onto the diseased tissue of a patient’s heart. Sawa says the patient moved out of intensive care within a few days. He plans to conduct the procedure in 8 more patients.
Work in animals shows that more cells tend to survive being transplanted in sheets or patches than when injected.
But studies have also found that such grafted cells do not beat in synchrony with the heart3. “If you put a patch on the surface, it marches to its own drum. It doesn’t hook up and keep pace with the rest of the heart muscle,” says Murry.
Researchers are also split on how the sheets work. Animal studies suggest that they might not create new muscle, but secrete growth factors that rejuvenate the existing heart tissue, a process known as the paracrine effect4.
Menasché plans to test this in people by only introducing the proteins the cells secrete. Whereas Zimmermann plans to test whether patches of cells supported by extracellular scaffolding create new muscle cells.
Zimmermann thinks that both injections and patches will be useful if they’re shown to work. Injection is more likely to help patients who have recently experienced a heart attack for whom surgery might not be appropriate, whereas patches could be used on those with chronic scarring in tissue where injected cells might not survive. “It will definitely not be case that one of the approaches will be the only one that is going to be useful,” he says. “There is no one size fits all approach.”
doi: 10.1038/d41586-020-01285-w
References
1.
Liu, Y.-W. et al. Nature Biotechnol. 36, 597-605 (2018).
PubMedArticleGoogle Scholar
2.
Shiba, Y. et al. Nature 538, 388–391 (2016).
PubMedArticleGoogle Scholar
3.
Gerbin, K. A., Yang, X., Murry, C. E. & Coulombe, K. L. PLoS One 10, e0131446 (2015).
PubMedArticleGoogle Scholar
4.
Zimmermann, W.-H. Curr. Opin. Physiol. 14, 70–77 (2020).
ArticleGoogle Scholar
5.
Funakoshi, S. et al. Sci. Rep. 6, 19111 (2016).
PubMedArticleGoogle Scholar

Leave a Reply