Scientists investigate how microbes in the nasal mucosa may influence the pathophysiology of chronic sinusitis Peer-Reviewed Publication
UNIVERSITY OF FUKUI
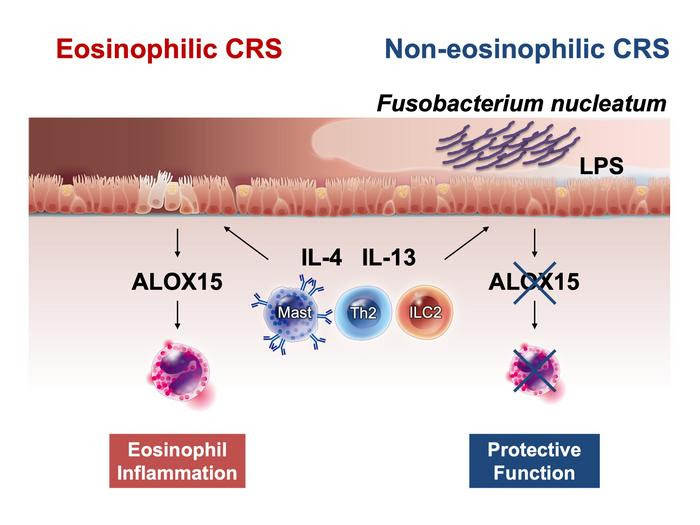
EXPERIMENTS CONDUCTED IN A RECENT STUDY BY RESEARCHERS FROM JAPAN SUGGEST THAT THE LIPOPOLYSACCHARIDES (LPS) PRODUCED BY THE BACTERIAL SPECIES F. NUCLEATUM SUPPRESSES THE EXPRESSION OF ALOX15 AND PREVENTS EXCESSIVE INFILTRATION OF EOSINOPHILS, WHICH CAUSES EOSINOPHILIC CRS, INTO NASAL CELLS.
view more
CREDIT: MASANORI KIDOGUCHI FROM UNIVERSITY OF FUKUI
Like other countries in the world, Japan has witnessed a worrisome increase in the prevalence of chronic rhinosinusitis (CRS) over the last decade. An inflammatory disease that lasts at least 12 weeks, CRS can cause nasal congestion, nasal discharge, trouble breathing through the nose, facial pain, and even loss of sense of smell. Unfortunately, treating CRS is complex since the disease manifests in various forms. CRS can be categorized into eosinophilic (ECRS) or non-eosinophilic (non-ECRS) types. In ECRS, the nasal and sinus tissues exhibit an increased presence of eosinophils, a type of white blood cell that releases inflammatory compounds.
The increased prevalence of CRS is largely driven by environmental factors that are in turn impacted by lifestyle changes. Of the several environmental factors, microorganisms residing in the nasal cavity and passages have been known to substantially affect our health. It is however, unclear whether the nasal microbiome contributes to the development of ECRS.
To address this knowledge gap, a research team from Japan led by Assistant Professor Masanori Kidoguchi from the Faculty of Medical Science of the University of Fukui, Japan, recently conducted a study on CRS in a Japanese population with a focus on the nasal microbiome. Their paper, which was also co-authored by Professor Shigeharu Fujieda from the University of Fukui and Professor Emiko Noguchi from the University of Tsukuba, was published in The Journal of Allergy and Clinical Immunology on September 25, 2023. Dr. Kidoguchi remarks, “We undertook this study because the pathological functions of bacteria and their metabolites in the development of ECRS remain unknown.”
First, the researchers collected nasal swabs from 143 subjects, of which 65 had ECRS, 45 had non-ECRS, and 33 were healthy control subjects. They then compared the microbiome diversity between the CRS and control groups from these samples and found significant differences, suggesting that the nasal microbiome is indeed involved in (or affected by) the disease.
More importantly, the microbiome composition differed significantly between the ECRS and non-ECRS groups. Through chemical and genetic testing, the team found that the bacterium Fusobacterium nucleatum (F. nucleatum) was less abundant in patients with ECRS. Furthermore, metagenomic analyses revealed that lipopolysaccharide (LPS) synthesis was greater in patients with non-ECRS than in those with ECRS.
Based on these results, Dr. Kidoguchi speculates, “F. nucleatum is known to cause inflammation by producing LPS. Some studies suggest that LPS has varying structures and functions depending on the bacterial species. We therefore hypothesized that LPS derived from F. nucleatum might be linked to the pathogenesis of both ECRS and non-ECRS.”
To test this hypothesis, the team investigated whether LPS isolated from F. nucleatum had an effect on the expression of specific cytokines in human bronchial epithelial cell cultures. Their experiments showed that LPS derived specifically from F. nucleatum suppressed the expression of ALOX15, an enzyme that plays a key role in the formation of nasal polyps and eosinophil-related inflammation.
Taken together, the results of this study reveal that disruptions in the nasal microbiome likely play a critical role in ECRS. This finding could be leveraged to develop more effective strategies to combat this troublesome condition. “The microbiome may strongly influence treatment resistance in CRS and may have an impact on other allergic diseases as well,” comments Dr. Kidoguchi, “Future studies will hopefully lead to probiotic development and lifestyle modification methods for preventing refractory chronic sinusitis.”
Let us hope a more thorough understanding of these inflammatory conditions would pave the way for treatments and prevention strategies that will improve the quality of life of patients with ECRS.
About University of Fukui, Japan
The University of Fukui is a preeminent research institution with robust undergraduate and graduate schools focusing on education, medical and science, engineering, and global and community studies. The university conducts cutting-edge research and strives to nurture human resources capable of contributing to society on the local, national, and global level.
Website: https://www.u-fukui.ac.jp/eng/
About Assistant Professor Masanori Kidoguchi from University of Fukui, Japan
Dr. Masanori Kidoguchi is an Assistant Professor of the Otorhinolaryngology, Head, and Neck Surgery Division at the University of Fukui. He obtained his Ph.D. in 2020 from the University of Fukui and has multiple research publications to his credit, with a special interest in otorhinolaryngology, immunology, allergy, and genomics.
Funding information
This study was funded by grants from the Japan Society for the Promotion of Science (KAKENHI grant no. 17H04344, 20K22998, 21H03086, and 21K16827), the Health Labour Sciences Research Grants program (grant no. H30-Nanchitou (nan)-Ippan-016), the Japan Agency for Medical Research and Development (grant no. JP22ek0410077h), and MSD Life Science Foundation, Public Interest Foundation (grant no. RA-017).
Media contact:
Naoki Tsukamoto
University of Fukui PR center
[email protected]
JOURNAL
Journal of Allergy and Clinical Immunology
DOI
10.1016/j.jaci.2023.06.029
METHOD OF RESEARCH
Experimental study
SUBJECT OF RESEARCH
People
ARTICLE TITLE
Nasal Microorganism to the Rescue? Study Confirms Protective Role of Bacterium in Chronic Rhinosinusitis
ARTICLE PUBLICATION DATE
25-Sep-2023
COI STATEMENT
S. Fujieda is an advisor for GlaxoSmithKline, Kyowa Kirin, and Sanofi; received honoraria from Kyorin Pharmaceutical, Taiho Pharma, and Mitsubishi Tanabe Pharma; and received research funding from Maruho, Tsumura, Mitsubishi Tanabe Pharma, and Sanofi. The rest of the authors declare that they have no relevant conflicts of interest

Leave a Reply